5 Didactic Day 5
Chris Walker: Shoulder Pain
Case
Chief Concern: Shoulder Pain
Take 13 minutes to obtain a history and negotiate a treatment plan with the patient.
When you complete your history, say, “I will now perform a physical exam” and then immediately say, “I have now completed the physical exam and it is consistent with the diagnosis of shoulder tendinitis.”
After the 13-minute interview, you will receive 13 minutes of feedback from the standardized patient educator, a student observer, and Family Medicine faculty.
There are no props…what you see is reality.
Patient with Autism Spectrum Disorder
Case
Chief Concern: Physical Exam
Take 13 minutes for your interview with the patient and parent (if present).
You will not perform a physical exam.
Follow instructions on the doorway information outside the room.
After the 13-minute interview, you will receive 13 minutes of feedback from the standardized patient educator, a student observer, and Family Medicine faculty.
Learning Objectives
- Describe how to approach a patient with autism
- Identify reasons autism is more prevalent than in the past
Required Reading: Autism: Why the Rise in Rates?
Required Reading: Autism: 5 Misconceptions That Can Complicate Care
Alma Pierce: Geriatrics
Case
Alma Pierce is an 80 year old female. She is brought in by her daughter-in-law Phyllis who is concerned. She has always been self-sufficient since her husband died 15 years ago. Phyllis has noticed a gradual decline in her function over the last few weeks. She has become more forgetful, somewhat lethargic, easily confused, has a poor appetite, and is unsteady on her feet. Phyllis emphasizes that this is not like her at all. She hopes that you can figure out what is wrong. Ms. Pierce has a sixth grade education.
Past Medical History:
- Mild systolic heart failure (40% EF on echo last year)
- Mild aortic stenosis (seen on last year’s echo)
- Chronic renal insufficiency (recent BUN/Cr= 31/1.6)
- Osteoporosis
- Anxiety
Medications: (There have been no recent medication changes)
- Lasix 20 mg BID
- KCl 20 mEQ daily
- Digoxin 0.25 mg daily
- Fosamax 70 mg weekly
- Lisinopril 20 mg daily
- Valium 5mg BID
- Aspirin 81 mg daily
Social history: Ms. Pierce lives in her own first-floor apartment and her daughter-in-law Phyllis lives upstairs and checks in on her a few times a day. She does not use alcohol, tobacco or drugs. She is not sexually active. She has been your patient for 20 years and you know her very well. Alma’s husband died 15 years ago. This was difficult for her at the time, but she was able to grieve appropriately with family support. She has a few friends who live nearby with whom she occasionally plays cards; otherwise she mostly stays at home. She loves to do crossword puzzles.
ADL’s/IADL’s: At baseline, Ms. Pierce is able to do all of her ADL’s independently (hygiene, continence, dressing, eating, toileting, and transferring). Phyllis helps with several of her IADL’s including driving, food shopping, finances, some meal preparation, and putting her medications into a weekly pill box. She has someone clean her apartment once a week. Alma is able to do some light cleaning and cooking on her own. Phyllis thinks that even in the last few weeks she has been taking all of her medications appropriately (they are gone from the pill box by the end of the week).
ROS: Ms. Pierce states she feels fine. She wonders what all the fuss is about! No headaches, blurry vision, falls (that Alma admits to, and Phyllis states that she has not witnessed any), no fever or chills, no belly pain, dysuria, emesis, diarrhea, constipation or blood in stool. No muscle aches or pains, no chest pain, no SOB. Occasional nausea. Phyllis states that she has been more tired then usual lately and is taking more naps. Phyllis thinks her appetite is decreased in the last week or so. She also says that she is forgetting things she does not usually forget; for example Phyllis tells her mother-in-law she will be coming down in an hour, and then Alma is surprised to see her. She is ambulating without difficulty, but seems a little less steady on her feet.
Learning Objectives
- Distinguish delirium from dementia
- Screen for delirium and cognitive impairment
- Describe harms of polypharmacy in the geriatric population and methods to reduce the harm
- Identify a resource about pharmacology in the elderly
Required Reading: Delirium
Required Reading: Deprescribing Is an Essential Part of Good Prescribing
Resource: Montreal Cognitive Assessment (MoCA): MOCA
Dermatology Workshop
Learning Objectives
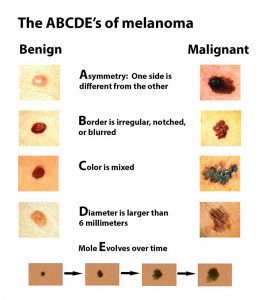
- Screen for melanoma
- Describe skin lesions
- Identify common skin conditions in children
Melanoma Screening:
harvardhealth.edu
Getting a Handle on Dermatology: Describing Skin Lesions
- LOCATION, LOCATION, LOCATION
- What is the involved body area?
- Confined to a discrete area, or diffuse?
- Is there involvement of face, palms, and soles?
- SIZE MATTERS
- If there are many lesions, what is the range in size?
- Are the lesions each discrete, or do they coalesce and become confluent?
- COLOR
- Flesh-colored, red (blanching or not), brown, black, varied, blue, pearly, etc.
- FLAT VS. RAISED
- Macule: a flat lesion (< 1cm) that you cannot feel
- Patch: a flat lesion (> 1cm) that you cannot feel
- Papule: a raised lesion (< 1cm) that you can feel
- Plaque: a raised lesion (> 1cm) that you can feel
- Nodule: a palpable lesion (< 2cm) within the dermis or subcutis (rather than in the epidermis)
- Tumor: a palpable lesion (> 2cm) within the dermis or subcutis (rather than in the epidermis)
- WELL-MARGINATED?
- A well marginated lesion transitions from normal to abnormal skin within 1 mm
- A poorly marginated lesion changes more gradually, taking more than 1 mm to transition from normal to abnormal skin
- BORDER
- Is the border of the lesion regular, or irregular in contour?
- EPITHELIAL DISRUPTION
- A smooth lesion without scale or crust is “without epithelial disruption”
- Lesions with epithelial disruption:
- Scaly Lesions: flakes of dry, whitish material caused by abnormal keratinization
- Crusted Lesions: due to dried secretions. May be black (from blood – eschar), yellow (serum) or green (pus)
- Hyperkeratotic Lesions: not scaly or crusted, but with an abnormal accumulation of the stratum corneum
- Erosions: moist, superficial skin defect involving only the dermis
- Ulcers: moist skin defect involving epidermis as well as deeper structures
- Vesicles: well marginated fluid filled lesion less than 1 cm in diameter
- Bulla: a vesicle over 1 cm in diameter
- Pustule: a vesicle containing purulent material
- MISCELLANEOUS
- Telangiectasias: fixed, visible dilated blood vessels within the epidermis
- Lichenification: accentuation of normal skin lines due to persistent rubbing or scratching
- Excoriation: erosion or ulcer caused by scratching, rubbing or picking
- Fissure: a linear split in the skin, through the epidermis and into the dermis
- Purpura: extravasated blood in the skin – usually purplish, often palpable, and non-blanching
Source: www.DermNetNZ.org
Readings
Required Reading: Common Skin Rashes in Children
Required Reading: Shave and Punch Biopsies
Required Reading: Dermatologic Conditions in Skin of Color, Part I
Required Reading: Dermatologic Conditions in Skin of Color, Part II
Optional Dermatology Resources
General Dermatology Websites:
1) DermNet New Zealand: Free online dermatology atlas: www.dermnetnz.org
2) Interactive Dermatology Atlas: Free online atlas, searchable by skin lesion characteristics, quiz mode: www.dermatlas.net
Dermoscopy Websites:
1) Introduction to Dermoscopy: PHARMAC NZ Seminar Series of about 10 lectures. Free. Lengthy, but comprehensive: https://www.pharmac.govt.nz/seminars/seminar-resources/dermoscopy/
2) Introduction to Dermoscopy for those who prefer written/image format rather than videos. Free.
https://www.dermnetnz.org/cme/dermoscopy-course/introduction-to-dermoscopy/
3) Dermoscopedia: Like wikipedia, for dermoscopy. Defines many terms. Free.
4) International Dermoscopy Society: Free membership, review of dermoscopy cases, international conferences: http://dermoscopy-ids.org
Free Dermoscopy App:
1) Dermoscopy Two Step Algorithm app. By Usatine. Free algorithm with images and photos to walk you through dermoscopic evaluation of skin lesions. Free.
Compiled by Amy L. Lee, MD
Wellness
Learning Objectives
- Define one’s own values and connect how they relate to wellness
- Create an action plan for maintaining wellness
Required Reading: Physician Burnout: Its Origins, Symptoms, and Five Main Causes
Optional Reading: Physician Resilience and Burnout: Can You Make the Switch?
Physician Wellbeing Worksheet
Tufts University School of Medicine, Department of Family Medicine
How do we work towards wholeness in our lives, as physicians and people? What would wholeness in our lives even look like? There are many areas of ongoing research and discussion about physician wellness, burnout, compassion fatigue, and finding meaning in our career in medicine. Here is a short personal worksheet to help you reflect on your own path to wellbeing, with some areas for personal notes, goals, and action plans.
1) Meaning: What is the reason you chose to become a physician, and what is the reason you continue to pursue medicine as a career? How can you stay connected with these reasons, as you go through your medical training?
_____________________________________________________________________________________________________________________________________________________________________________
2) Values: What is most important to you in your life? These things might change throughout your life, but some might be constant. How are you prioritizing these values in your life right now? How do you plan to prioritize them in the future?
My Top 5 Values
- __________________________
- __________________________
- __________________________
- __________________________
- __________________________
3) Self Care: How do you take care of your body, your mind, your heart and your spirit? Is this a priority for you? Studies show that doctors who care for all these aspects of themselves and prioritize self care are happier and more resilient; and their patients have better health outcomes. What are you doing now, and what can you do in the future, to care for yourself?
________________________________________________________________________________________________________________________________________________________________________________
4) Planning: Physician wellbeing and happiness do not happen by chance. Planning, reflection, and regular re-evaluation are necessary to continually adjust as we pursue the goals of a meaningful and fulfilling career and a happy life.
Some Questions to Ponder
-Where do I see myself in the future? In 5 years? 10 years?
-What is most meaningful to me in life and in medicine, and how do I maximize that meaning in my daily life?
-How do I line up my values with my career?
-Have I found any physicians who I want to be like? What are they doing to pursue wholeness?
__________________________________________________________________________________________________________________________________________________________________________________
Action Plan Ideas
- Find a physician mentor that seems happy. Talk to them about how they got where they are and how they structure their career and life.
- Talk to your support system (family/friends who know you well) about your values and plans.
- Consider the meaning behind your choice to go into medicine, and how you can connect with that meaning on a regular basis.
- Think about what you can do now to get on your desired path.
- Establish lifetime habits to enhance your wellbeing and happiness.
- Start or maintain or increase self-care.
Your Personal Action Plan
- ____________________________________________________
- ____________________________________________________
- ____________________________________________________
- ____________________________________________________
- ____________________________________________________
Last edit by Amy L. Lee, MD 4/2018
Important Information Concerning Mental Health Resources
at Tufts University School of Medicine
Did you know that there are resources for students to discuss mental health issues at TUSM? There is the free Talk One2One Program – see information below. Also, Sharon “Snaggs” Gendron is the Student Wellness Advisor. She can be reached at Sharon.Snaggs@tufts.edu or you can stop by the Health Administration office:
Monday thru Friday:
Posner Hall, Room 406
200 Harrison Avenue
Boston, MA 02111
PH: (617) 636-2700
Students should feel free to come by and talk. Outside referrals can be provided as well.
You can obtain more information about the Health Administration office at: medicine.tufts.edu/saha.
Medical school can be quite challenging. You may feel academically or personally overwhelmed,
lonely, saddened by events in your life. You may be far away from family, uncertain about your
future plans, or you may want to take some time away from studying to chat with someone.
This resource is completely confidential.
ADDITIONAL RESOURCES
You are invited to check out the blog started by TUSM FM faculty Dr. Amy L. Lee, focused on physician wellbeing:

WORKING TOWARDS WHOLENESS IN OUR LIVES, AS DOCTORS AND PEOPLE
Join the conversation, read the blog, connect with faculty and other students in the health professions at:
Yoga (for Didactic Day 6)
Required Article: Exercise, Yoga, and Meditation for Depressive and Anxiety Disorders
