Introduction
Jump to: Clerkship Calendar, Grading, Assignments, Electives, Genograms
Family Medicine Clerkship Objectives
Clerkship Goals
At the end of the Family Medicine Clerkship, the successful student will be able to:
- Discuss the value of primary care to any health care system.
- Assess a patient, formulate a differential diagnosis, and use critical thinking to propose a patient-centered management plan for patients with common acute presentations.
- Manage a chronic illness follow up visit for patients with common chronic diseases.
- Develop an evidence-based health maintenance plan for a patient of any age or gender.
- Demonstrate advanced communication skills in history-taking and counseling patients.
- Perform both focused and complete physical exams.
- Describe the critical role of a patient’s family, social network, and culture in diagnosing and treating illness.
- Identify the principles of Family Medicine Care: continuity, comprehensiveness, coordination, community, prevention, and family.
- Use principles of collaborative interprofessional team-based care.
- Apply the principles of Information Mastery.
| Objective | Level of Competence | Evaluation Method | ACGME Competency |
| 1. The role of Primary Care in an Effective Health Care System (Goals 1, 9) | |||
| Identifies the connection between a health care system with a strong primary care base and better outcomes for lower costs on a population level. | K | MCQ | SBP |
| Identifies the connection between a health care system with a strong primary care base and decrease in health disparities. | K | MCQ | SBP |
| Demonstrates the importance of team-based care by collaborating with non-physician health members of the health care team. | D | DO | SBP |
| 2. Enhanced Role of the Medical Student (Goals 2, 3, 5, 6) | |||
| Exercises autonomy with patients and is involved in care for a high volume of patients. | D | DO | PC |
| Distinguishes between normal and abnormal findings. | KH | DO | MK |
| Demonstrates level-appropriate confidence in patient communication and care management. | D | DO | PC |
| 3. The Patient-Physician Relationship (Goals 2, 5, 7, 8, 9) | |||
| Collaborates with patients and families to establish a therapeutic partnership by exploring the patient’s perspective, identifying a mutual agenda, establishing common ground for treatment. | D | DO | ICS |
| Demonstrates insight as to how one’s personal biases impact the care of patients. | K | online exercise | P |
| Identifies the connection between continuity in patient care, and improved care via enhanced trust and skill at behavioral change strategies. | K | DO | SBP |
| 4. History and Physical Exam: advancing skills from the foundation years (Goals 5, 6) | |||
| Elicit a focused history appropriate for the ambulatory setting. | D | DO | PC |
| Performs a focused exam appropriate for the ambulatory setting. | D | DO | PC |
| Presents history and physical to attending in an organized and succinct fashion. | KH | DO | MK |
| 5. Common Illness and Presentations Across the Life Span (Goals 2, 3, 4) | |||
Demonstrates competence with the diagnosis and management of common medical problems (pertaining to all age groups) including, but not limited to:
|
KH | DO, MCQ | MK |
| 6. Information Mastery (Goals 2, 3, 4, 10) | |||
| Efficiently finds high quality evidence at the point of care | D | CP | PBLI |
| Demonstrates academic curiosity necessary for life-long learning | D | CP, DO | PBLI |
| 7. Counseling: Utilizing advanced communication skills, motivational interviewing and empowerment to bring about positive change for patients (Goals 3, 5, 7) | |||
| Use Stages of Change model and counsels patients in areas including tobacco, substance abuse, medication/immunization adherence, and high-risk sexual behaviors | KH | DO, MCQ, SP | ICS |
| Demonstrates appropriate counseling techniques about nutrition for a variety of common illnesses, such as obesity, diabetes mellitus, hyperlipidemia and hypertension | KH | DO, MCQ, SP | ICS |
| 8. Patient-Centered Care (Goals 1, 5, 7, 8) | |||
| Applies understanding of patients’ life circumstances, such as family, community, finances, work, education, spirituality, and culture, when establishing an assessment and plan | D | DO, SP | ICS |
| Screens patients for interpersonal violence | D | DO | ICS |
| Performs a home assessment on a patient | D | CP | PC |
| 9. Ambulatory Procedures (Goal 1) | |||
| Develops basic competency in at least 5 procedures | |||
|
D | DO | PC |
| 10. Documentation and the Electronic Medical Record (Goals 2, 3, 4, 6) | |||
| Effectively uses the electronic health record to document patient encounters and to extract data | D | DO | MK |
| Documents appropriately and in an organized fashion for episodic visits, chronic disease management, and health maintenance | D | DO | MK |
Extensive details about each curricular area can be found in the STFM Family Medicine Clerkship Core Curriculum.
Key to Abbreviations
| Levels of Competence Abbreviations
K = Knows KH = Knows How SH= Shows How D = Does
|
ACGME Competency Abbreviations
PC = Patient Care MK = Medical Knowledge PBLI = Practice-based Learning & Improvement ICS = Interpersonal & Communication Skills P = Professionalism SBP = Systems-based Practice |
Method of Evaluation and ACGME Toolbox of Assessment Methods
| Chart Review (CR)
Direct Observation (DO) Simulated Patient (SP) Multiple Choice Examination (MCQ) Objective Structured Clinical Exam (OSCE) Case Presentation (CP) Oral Exam |
What is Family Medicine?
From the American Academy of Family Physicians:
In the increasingly fragmented world of health care, one thing remains constant: family physicians are dedicated to treating the whole person. Family medicine’s cornerstone is an ongoing, personal patient-physician relationship focusing on integrated care.
Unlike other specialties that are limited to a particular organ or disease, family medicine integrates care for patients of all genders and every age, and advocates for the patient in a complex health care system.
The AAFP represents 129,000 physicians and student members nationwide. It is the only medical society devoted solely to primary care. Family physicians conduct approximately one in five office visits — that’s 192 million visits annually – 48 percent more than to the next most visited specialty.
The specialty of family medicine was created in 1969 to fulfill the generalist function in medicine, which suffered with the growth of subspecialization after World War II. Since its creation, the specialty has delivered on its promise to reverse the decline of general medicine and provide personal, front-line medical care to people of all socioeconomic strata and in all regions of the United States.
Today, family physicians provide the majority of care for America’s underserved rural and urban populations. In fact, family physicians are distributed more proportionally to the U.S. population than any other physician specialty. Without family physicians, rural and underserved populations, in particular, would lack access to primary care.
Because of their extensive training, family physicians are the only specialists qualified to treat most ailments and provide comprehensive health care for people of all ages– from newborns to seniors. Like other medical specialists, family physicians complete a three-year residency program after graduating from medical school.
As part of their residency, they participate in integrated inpatient and outpatient learning and receive training in six major medical areas: pediatrics, obstetrics and gynecology, internal medicine, psychiatry and neurology, surgery, and community medicine. They also receive instruction in many other areas including geriatrics, emergency medicine, ophthalmology, radiology, orthopedics, otolaryngology, and urology.
Family physicians deliver a range of acute, chronic, and preventive medical care services while providing patients with a patient-centered medical home.
In addition to diagnosing and treating illness, they also provide preventive care, including routine checkups, health-risk assessments, immunization and screening tests, and personalized counseling on maintaining a healthy lifestyle. Family physicians also manage chronic illness, often coordinating care provided by other subspecialists. From heart disease, stroke and hypertension, to diabetes, cancer, and asthma, family physicians provide ongoing, personal care for the nation’s most serious health problems.
More reading:
Patient information about what family doctors do can be found at this website.
Here is a link to one description about some differences between Family Medicine and Internal Medicine vis a vis their training programs (residencies). One additional difference not highlighted in this reading is that Family Medicine training heavily emphasizes behavioral health.
Structure of the Rotation
During the 6 weeks, you will spend on average 4 days a week at your assigned clinical site. One day a week (on average) is spent back at Tufts in a day-long (8:30am – 5:00pm) classroom based session (“didactic days”).
We truly value student feedback on the didactic days. Therefore, before leaving each didactic day at 5pm, please submit your anonymous evaluation for the day.
FM Clerkship Clinical Encounter (Patients) Table
Students are required to see a minimum of one patient in each category listed below. Student are required to log all patients seen who fall into the categories listed below. For example, students should log all patients seen with depression and anxiety. The clinical problems and diagnoses should be active issues for the patient. More than one problem or diagnosis may be logged for a single patient. Logs are on TUSK.
| Types of Patients to be seen | Level of Student Responsibility | Alternative Clinical Learning Experience |
| EVALUATION OF A PATIENT WITH: | ||
| Depression/Anxiety | AP | DD (Didactic Day) |
| Rash/Skin Cancer | AP | DD, TUSK reading |
| Respiratory Tract Infection | AP | DD, Syllabus |
| Hypertension | AP | DD, Syllabus |
| Diabetes Mellitus | AP | DD, Syllabus |
| Hyperlipidemia | AP | DD or FM Cases |
| Cardiovascular Disease | AP | DD or FM Cases |
| Musculoskeletal Issue | AP | DD |
| Complete Physical/Health Maintenance/Prevention | AP | DD, FM Cases |
| Asthma/Dyspnea/Cough | AP | DD |
| Women’s Health | AP | DD, Syllabus |
| Pediatric Issue | AP | DD or FM Cases |
| Geriatric Issue | AP | DD or FM Cases |
| Headache or Dizziness | AP | FM Cases |
| Chronic or Acute Pain | AP | DD or FM Cases |
| Fatigue/Insomnia | AP | DD or FM Cases |
| Abdominal Pain/Gastrointestinal Complaint | AP | DD or FM Cases |
| Intimate Partner Violence | AP | DD or FM Cases |
| INFORMATION MASTERY | ||
| Finds high quality evidence at point of care to assist preceptor in clinical decision making | AP | DD, Info Mastery assignment |
| LIFESTYLE MODIFICATION COUNSELING | ||
| Nutrition | AP | DD, SP Exercise |
| Exercise | AP | DD |
| Alcohol | AP | DD |
| Tobacco | AP | DD |
| Drug Use | AP | DD |
| Medication/Immunization Adherence | AP | DD |
| COMMUNICATION | ||
| Focused History | AP | CAP |
| Focused Exam | AP | CAP |
| Complete Exam | AP | CAP |
| Oral Presentation | AP | CAP |
| Written Documentation | AP | CAP |
| Team-based care: collaborated with non-physician member of health care team | AP | DD |
| PROCEDURES | ||
| Pelvic/Gynecologic Exam | AP or OB | CAP |
| Derm Procedure or Cryotherapy | AP or OB | DD |
| PATIENT-PHYSICIAN RELATIONSHIP | ||
| See a patient a second time | AP | CAP |
| Elicit patient’s perspective | AP | DD |
| Collaborate with patient | AP | DD |
| Motivational Interviewing | AP or OB | DD |
OB = Observation, AP = Active Participation (took some components of history and physical examination and engaged in clinical reasoning)
Clerkships: M = Medicine, N = Neurology, O = OB/GYN, P = Pediatrics, S = Surgery
CAP = Competency-based Apprenticeship in Primary Care (prerequisite for enrollment in 3rd year clerkship)
Students are required to see the following number of patients:
Minimum number of patients worked up per week: 10
Minimum number of patients observed per week: 5
Top 10 Ways To Be Helpful To Your Preceptor
1. Provide Patient Education
Offer to review your preceptor’s plan with the patient (after the preceptor leaves) to make sure the patient understands; write it down if necessary
Find an appropriate handout online and go through the handout with the patient
2. Research the latest evidence on clinical questions that come up with patients each day
Succinctly give evidence on a clinical question to your preceptor in the exam room, in real time
You can even teach your preceptors how to do this if they wish (if they need a password to the TUSM library, put them in touch with us and we will help them)
3. Write notes
Learn how your preceptor likes to document and write as much of the note as possible
4. Counsel patients
Nutrition, exercise, smoking cessation, alcohol, safe sex, asthma, contraception…
5. Geriatric Evaluation
MoCA, IADLs/ADLs, Depression Screen
Home Visit
6. Patient medications and/or instructions
Reconcile Medications
Write out list of medications for patients with the reasons they are taking them
7. Call patients
Give lab results
Answer their questions
Check in on them
8. Help staff
Bring patients back to exam rooms/take vitals
Look for other ways to be helpful
9. Learn how to present patients in a succinct and organized manner, the way your preceptor(s) like it. Encourage your preceptors to let you present in front of the patient. This benefits:
Doctor: spends time with the patient instead of in a back office with only the student. Very efficiently can educate student and patient simultaneously.
Patient: confirms that the entire story has been relayed properly, and is delighted to hear the thought process used to arrive at their diagnosis and treatment plan.
Student: gets to practice communicating without using medical jargon.
10. Busy yourself! When your preceptors need a moment of quiet time, try to busy yourself, either with work related to your preceptor’s office, or with reading material so as not to burden your preceptors with the feeling that they need to entertain you.
Family Medicine Clerkship Calendar
| Monday | Tuesday | Wednesday | Thursday | Friday | |
| Week 1 | Didactic Day 1 (8:30-5:00), TUSM Clerkship Orientation Information Mastery Fatigue Pain Antibiotics Health Maintenance |
Report to Preceptor | Didactic Day 2 (8:30-5:00), TUSM Adolescent Health Child with Cough Upper Respiratory Infection Immunizations Diabetes Mellitus Women’s Health Workshop: Intimate Partner Violence, Maternity Care, Menopause, Contraception Hypertension |
||
| Week 2 | PACT Table due by DD3 | Watch video (link in email) | Didactic Day 3 (8:30-5:00), Tufts Family Medicine Residency in Malden PACT Table Due Alcohol, Tobacco Motivational Interviewing Health Systems Nutrition Pregnancy Options Sports Medicine Workshop: Shoulder, Knee, Ankle, Elbow, Foot, Wrist |
||
| Week 3 | Didactic Day 4 (8:30-4:30), Lawrence Family Medicine Residency Serving Underserved /Community Health Center Global Health and Obstetrics Transgender Care Money and Medicine HIV and Primary Care Caring for the Homeless Group Visits and Empowerment |
Mid-Clerkship Evaluation: Complete self-evaluation & give to preceptor for discussion & signature. Hand in by DD5. Info Mastery Exercise (IME) topic due in Canvas by Tuesday, week 4. |
|||
| Week 4 | IME Topic Due (in Canvas) | ||||
| Week 5 | 3 DOC Cards (1 Pain + 2 more) and Clinical Reasoning Tool due by DD5 16 FM Cases due by DD5 Home Visit due by DD5 5 Wishes Reflection due by DD5 |
Didactic Day 5 (8:30-5:00), TUSM Mid-Clerkship Evaluation Due 3 DOC Cards (1 Pain + 2 more)DueClinical Reasoning Tool Due 5 Wishes Reflection Due 16 FM Cases Due Home Visit Due Info Mastery Presentations Standardized Patients Geriatrics End of Life DebriefPhysician Wellness Dermatology Workshop |
|||
| Week 6 | >75 Patient logs due by DD6 | Extra Credit due by DD6 | Final eval with preceptor (nothing due for this) | Didactic Day 6 (8:30-12:00), TUSM Exam Yoga |
Directions to Residencies
Didactic Days 3 and 4
Tufts Family Medicine Residency
at Cambridge Health Alliance
195 Canal Street, Malden, 781-338-0500
From Boston:
Take Route 93 North to Exit 29/Somerville/Everett. The exit forks. Stay right on 28N/Everett/Malden. In less than a mile, you will get to a huge intersection where you will go straight, following signs to stay on 28N. Go about 1 more mile and at a light, take a right on Medford Street. Go thru 3 lights and at the 4th light, take a left on Canal St. The Tufts Family Medicine Residency is about 0.1 miles ahead on the left. Use the larger parking lot after the building and park in the blue spaces (white spaces reserved for patients and staff).
Lawrence Family Medicine Residency
34 Haverhill Street, Lawrence, 978-725-7410
From Boston:
93 North, about 20 miles to 495 North, about 5 miles to Exit 44-45, Marston St. take the long exit ramp that goes under 495 and directly onto Marston St. which turns into Prospect St. 3/4 mile after leaving exit ramp, you’ll see Lawrence General Hospital on the left. Go 2/10 mile past the hospital and take a sharp left (first left after hospital) onto Haverhill St. Health Center is #34 down the hill on the left.
Take the elevator to the third floor and follow the sign to the appropriate conference room.
Feedback, Evaluation, and Grading
| Preceptor Evaluation | 55% |
| Exam | 25% |
| Information Mastery Exercise | 10% |
| Didactic Day Performance | 10% |
| Honors | 91.50 – 100 |
| High Pass | 81.50 – 91.49 |
| Pass | 70.00 – 81.49 |
| Low Pass | 60.00 – 69.99 |
Orientation/Expectations: Please complete the Family Medicine Clerkship Preceptor Introduction Form prior to meeting with your preceptor. Meet with your preceptor at the beginning of the rotation so that you can communicate your goals for the clerkship. At that time, your preceptor will share his/her expectations of you.
Mid-Clerkship Evaluation: At the end of the third week of the clerkship, meet with your preceptor to discuss your progress noting how expectations are being met. At this point, develop strategies for the remainder of the clerkship. Have your preceptor sign your Mid-Clerkship Evaluation Form and return it along with 3 DOC cards (including the Pain DOC Card) by DD5.
Final Evaluation: At the end of the clerkship, your preceptor will meet with you for your final evaluation. S/he will complete an online evaluation that will make up 55% of your clerkship grade. You will be asked to evaluate your preceptor after the clerkship. Your preceptor does not see this evaluation until after your final grade has been submitted. If you receive a clinical grade of Low Pass, your final grade cannot be higher than a Low Pass. If you receive a clinical grade of Fail, your final grade will be Fail. A student with a clinical grade of Low Pass or Fail will automatically be reviewed by the TUSM Student Ethics and Promotion Committee regardless of their written exam score. A student with a clinical grade of Low Pass who fails the exam will receive a final grade of Fail for the clerkship and will automatically be reviewed by the TUSM Student Ethics and Promotion Committee.
Family Medicine Clerkship Exam: The FM Clerkship Exam makes up 25% of your grade. The content of the exam comes from patients you see and read about in the Family Medicine setting, and the Family Medicine Clerkship Syllabus. Most major concepts are discussed during the didactic sessions. The exam consists of 2 parts (see Exam details for more information). Students must achieve 65% on part 1, 60% on part 2, and 65% for the total exam grade in order to pass. Students who fail the exam will be given one chance to remediate the exam. The score of the first exam will be used to calculate the overall clerkship grade. If a student fails the exam a second time, s/he will not pass the clerkship and the first exam score will be used to calculate whether s/he receive a Low Pass or Failing grade. Retake exams are generally scheduled within 6 weeks to 3 months from when the initial exam results are reported. Any exceptions to this time frame must be approved by the Dean of Students. Click on the Family Medicine Clerkship Exam link for a more extensive description and some sample exam questions.
Information Mastery Exercise: The Information Mastery Exercise makes up 10% of your grade.
fmCases: Students must complete 16 fmCases (https://aquifer.org) in order to pass the FM Clerkship. Eight cases are required, and eight may be chosen from the remaining options. If a student’s record indicates that an unreasonable amount of time was spent on the case, credit will not be given for that case. Students will not be given credit for cases they have already completed in previous clerkships. If one of the 8 required cases has already been completed on a prior clerkship, students should complete any other case of their choosing. Required Cases: #7, 9, 12, 18, 19, 27, 28, 33, plus eight more of student’s choice.
Patient Logs: Students are required to complete a minimum of 75 Patient Logs in order to pass the FM Clerkship.
Home Visit Assignment, Five Wishes Assignment, PACT Culture Assignment: Five points will be deducted from your final grade for each incomplete assignment.
9-10: Perfect attendance, punctuality; exceptional insight and participation; advanced understanding of patient-centered care
6-8: Excellent attendance and punctuality; good insight and participation; good understanding of patient-centered care
3-5: Instance(s) of poor attendance and/or punctuality; poor-adequate insight and participation
0-2: Poor attendance and punctuality; lack of insight and/or participation
FM Clerkship Grading Criteria
1. Knowledge for Practice: Demonstrates knowledge of common illnesses and presentations across the lifespan, including the diagnosis and management of such problems. Applies established and emerging principles of clinical science to diagnostic and therapeutic decision-making, clinical problem solving, and other aspects of evidence-based care.
2. Knowledge for Practice Comments:
3. Patient Care/Clinical Skills – History: Obtains an accurate medical history that covers all essential aspects for the primary care setting. Takes history in a logical, organized and focused manner. Screens patients for sensitive issues such as alcohol use, interpersonal violence and depression.
4. Patient Care/Clinical Skills – History Comments:
5. Patient Care/Clinical Skills – Physical Exam/Basic Procedures: Performs both a complete and problem-focused physical examination appropriate for the primary care setting and accounting for patient age and presentation. Shows sensitivity to privacy and modesty during exam. Performs routine technical procedures appropriate to primary care.
6. Patient Care/Clinical Skills – Physical Exam/Basic Procedures Comments:
7. Patient Care/Clinical Skills – Information Mastery:
Identifies high-quality evidence to assist in clinical decision-making. Effectively communicates this evidence to patients.
8. Patient Care/Clinical Skills – Information Mastery Comments:
9. Patient Care/Clinical Skills – Clinical Reasoning:
Identifies pertinent history and physical exam findings that are useful in diagnosis of core illnesses. Interprets the results of commonly used diagnostic procedures and tests. Reasons deductively about diagnostic and therapeutic interventions for patients with common conditions and constructs an appropriate differential diagnosis. Demonstrates an investigatory and analytic approach to clinical situations. Detects clinical scenarios that are potentially life threatening and describes how to institute appropriate therapy. Applies shared decision-making when formulating assessments and plans.
10. Patient Care/Clinical Skills – Clinical Reasoning Comments:
11. Communication Skills (patient): Establishes and maintains rapport and therapeutic relationships with patients and families. Counsels patients effectively and non-judgmentally via advanced communication skills. Demonstrates respect, empathy, cultural sensitivity. Uses lay language and avoids medical jargon. Participates in shared decision-making in patient-centered care. Communicates effectively with patients of all ages, abilities, gender identities, races, ethnicities, sexual orientations, levels of health literacy, and socioeconomic classes. Demonstrates sensitivity, honesty, and compassion in difficult conversations, including those about death, end of life, adverse events, bad news, disclosure of errors, and other sensitive topics. If applicable, works effectively with a medical interpreter for a patient whose preferred or primary language is not English.
12. Communication Skills (patient) Comments:
13. Oral Communication Skills (colleagues/peers): Demonstrates effective communication with the health care team. Presents oral case presentations in a clear, concise, articulate, accurate manner. Gives and accepts constructive feedback to/from other members of the health care team.
14. Oral Communication Skills (colleagues/peers) Comments:
15. Written Communication Skills (colleagues/peers): Effectively uses the electronic health record. Writes clear, concise and well-organized notes as appropriate for episodic visits, chronic disease management and health maintenance.
16. Written Communication Skills (colleagues/peers) Comments:
17. Professionalism: Demonstrates an appropriate professional manner (including but not limited to attendance, punctuality, physical appearance, dress, patient confidentiality, and responsible use of technology and social media). Demonstrates accountability, honesty and integrity. Demonstrates compassion for patients/families and respect for their privacy and dignity. Demonstrates a commitment to ethical principles pertaining to the doctor-patient relationship, confidentiality, informed consent, and relevant compliance or business practices. Demonstrates commitment to the welfare of one’s patient as one’s primary professional concern.
18. Professionalism Comments:
19. Practice Based Learning and Improvement: Demonstrates interest in learning. Acknowledges own deficiencies and makes sincere effort to improve; asks and accepts feedback. Demonstrates effective self-directed learning skills, including the ability to reflect on, act upon, and reassess one’s professional performance. Educates other health professionals. Acknowledges and manages uncertainty in clinical care.
20. Practice Based Learning and Improvement Comments:
21. Systems Based Practice: Identifies the family physician’s role in coordinating care of the patient and in improving outcomes, decreasing health disparities and controlling costs on a population level. Describes medical costs and their impact on individual and population health. Critically evaluates quality and safety practices.
22. Systems Based Practice Comments:
23. Interprofessional Collaboration: Respects the unique cultures, values, roles/responsibilities, and expertise of other health professions. Listens actively, communicates respectfully and encourages ideas and opinions of other team members. Applies knowledge of the roles and responsibilities of other health care professionals and how the team works together to provide patient care. Reflects on individual and team performance.
24. Interprofessional Collaboration Comments:
25. Personal and Professional Development. Uses healthy coping mechanisms to respond to stress. Manages the tension between personal and professional responsibilities. Practices responsibility, integrity, flexibility and maturity in adjusting to change, with the capacity to alter one’s behavior. Demonstrates trustworthiness in autonomous care of a patient. Asks for help when appropriate.
26. Personal and Professional Development Comments:
27. Evaluator’s Formative Comments on Student Performance: Provide the student with specific suggestions and directions for further learning and development. Comments of concern noted here will be brought to the Dean of Students’ attention.
28. Evaluator’s Summary Comments on Student Performance: Comments for potential use in the Dean’s Letter. These comments should note specific examples or anecdotes of particular strengths, weaknesses or inconsistencies in the student’s performance.
HONORS: Outstanding overall performance, well beyond expectations: comprehensive knowledge base, utilizes evidence effectively with regard to clinical decision-making; outstanding patient care/clinical skills; outstanding communication/ interpersonal skills; demonstrates a zeal for learning and self-improvement; consistently meets highest standards of professional conduct and behavior.
HIGH PASS: Excellent overall performance, meets and often exceeds expectations: strong knowledge base, very good to excellent patient care/clinical skills; very good to excellent communication/ interpersonal skills, eager to learn, sound clinical reasoning, meets high standards of professional conduct and behavior.
PASS: Adequate overall performance, meets all expectations: Adequate fund of knowledge and reasonable clinical decision skills; good patient care/clinical skills, adequate interpersonal skills; able to respond to feedback and shows self-improvement; meets standards of medical professionalism.
LOW PASS: Marginal performance; does not consistently meet expectations in all domains: May demonstrate limitations in any of the following areas: knowledge base, clinical decision-making; organizational skills; communication/interpersonal skills; level of interest/initiative; response to feedback/self-improvement. Does not consistently meet standards of medical professionalism. For promotion and graduation, conditions outlined by Promotions Committee must be satisfied.
FAIL: Exceptionally poor performance, does not meet expectations: Serious unacceptable deficiencies in one or more domains: does not accept responsibilities; insufficient fund of knowledge; inadequate clinical skills; ineffective communication skills; not always sensitive to patient’s needs, disorganized; unprofessional behavior. For promotion and graduation, conditions outlined by Promotions Committee must be satisfied.
Attendance Policy
Due to illness or other emergency, students may be granted ONE (1) excused absence during the rotation without needing to make up the day. More than one day missed for excused absences must be made up clinically.
An excused absence MUST be excused through the clerkship director and/or the Dean’s office. A site preceptor cannot excuse a student.
Excused absences are typically granted only for illness or other serious emergency. Attending a wedding, presenting at a conference, and other worthy endeavors do NOT constitute excused absences and students may not miss clinical obligations for these reasons even if they offer to make up the time. There are no personal days during the clinical years. Please note, students have 6 weeks of vacation during 3rd year outside of rotation time.
Preceptors report if and how many days their student(s) missed on the final evaluation form.
Didactic days are mandatory.
FM Clerkship Elective Opportunities
Some students will wish to explore a facet of Family Medicine not available at their primary clerkship site. Below are multiple half-day opportunities to experience specialized aspects of Family Medicine at other locations. These “field trips” are optional.
You will be allowed to participate in up to two of these electives. You do not have to do any of them. Read through them and rank your top 5 choices if you are interested.
| Obstetrics in Family Medicine | |
| Kathe Miller, MD | T: (617) 665-1117 |
| Cambridge Health Alliance Dept. of Family Medicine | Email: hsimone@challiance.org |
| Available only on Saturdays |
Spend a Saturday or a Sunday on call with a family doctor on Labor and Delivery at the Cambridge Hospital. Your activities may include postpartum and newborn rounding, labor triages and management of laboring patients, depending on what is happening in the hospital that day.
| Sports Medicine | |
| Warren Bodine, DO | Email: warren.bodine@glfhc.org |
| 34 Haverhill Street, Lawrence | Lawrence Family Medicine Residency Program |
During this elective you will spend one half day with Dr. Warren Bodine, a Board Certified Osteopathic Family Physician and Primary Care Sports Medicine Physician during his sports medicine clinic. You will be exposed to the assessment and treatment of sports-related and other musculoskeletal injuries such as fractures, sprains, and strains. You will learn about sports physicals and concussion management as well as joint and bursa injections. This elective is intended to give you an appreciation of Family Medicine/Sports Medicine, its approach to patient care, and the care of athletes at all scopes and levels.
| Transgender Care | |
| Josh St. Louis, MD | Email: joshua.stlouis@glfhc.org |
| 34 Haverhill Street, Lawrence | Lawrence Family Medicine Residency Program |
Join Dr. St. Louis in his practice in Lawrence to learn about health care for transgender patients in a community health center. Email him to set up a mutually convenient time.
| Integrative Medicine | |
| Andrea Gordon, MD | Email: agordon@challiance.org |
| 195 Canal Street | Tufts Family Medicine Residency Program |
| Malden, MA 02148 | Wednesdays 9am – 12:30pm |
During this elective you will spend a half day in an integrative medicine clinic. You will experience non-allopathic approaches to healthcare such as osteopathic manipulation, nutrition, herbal medicine, energy medicine and lifestyle suggestions. You will also be exposed to online integrative medicine resources. This elective is intended to give you an appreciation of Family Medicine/Integrative Medicine and its role in holistic patient care.
| Osteopathy/Integrative Medicine | |
| Darcy Thomas, DO | T: (978) 873-6572 |
| Osteopathic Family Medicine, 22 Mill Street Ste 201 | Email: darcythomasdo@gmail.com |
| Arlington, MA 02476 | Tuesdays |
This elective focuses primarily on the practices and principles of osteopathic medicine, a practice of medicine started by Dr. Andrew Taylor Still in the late 1800’s. It incorporates the idea of focusing on health rather than disease. You will learn about the osteopathic principles while getting to experience and practice some hands-on techniques to treat various medical conditions. Trigger point injection with acupuncture needles (dry needling) as well as nutrition with ayurvedic principles may be used as well, depending upon each patient’s needs. This elective is best for those who are open to alternatives.
| Academic Family Medicine | |
| Allen Shaughnessy, Pharm.D., M.Med.Ed. | T: (617) 694-8817 |
| Tufts Family Medicine Residency Program | Email: ashaughnessy@challiance.org |
| 195 Canal Street Malden, MA 02148 | Monday afternoons |
You will join a three-hour academic discussion at the Tufts University Family Medicine Residency Program Master Teacher Fellowship. Topics vary but may include curriculum design, program design, teaching techniques, information mastery, educational theory, adult learning, assessment, or mentoring. At this meeting, you will meet fellows and attendings who teach at the residency and medical school level, and you will get the opportunity to ask them questions about a career in academic family medicine.
| Direct Primary Care |
|
| Carmela Mancini, DO, MPH | T: 781-842-3961 |
| Gold Direct Care | Email: drmancini@golddirectcare.com |
| 123 Pleasant St, Marblehead, MA 01945 | Wednesday or Thursday |
Learn about Direct Primary Care, a privately owned practice that does not contract with insurance companies at all, giving patients personalized and direct access to their doctors.
| Functional Medicine/Direct Primary Care | |
| Jeffrey Wacks | Email: info@patriotdirectfm.com |
| 117 W Central Street | 508-318-6941 |
| Natick, MA 01760 | Contact to set up day & time |
Functional Medicine/Direct Primary Care with Dr. Jeffrey Wacks.
| Abortion Care | |
| Honor MacNaughton, MD | Email: homacnaughton@challiance.org |
| Cambridge Health Alliance | Wednesdays 3-8pm |
You will spend one half day with a family physician and reproductive health and advocacy fellow who provides full-spectrum reproductive health services in the outpatient setting. You will be exposed to options counseling for unintended pregnancy, contraceptive management, and first trimester abortion care. Learn about the range of family planning services that can be offered by family physicians. Interested students will have the opportunity to ask about providing reproductive health care in their future practices.
| Wellness Group Visits | |
| Wayne Altman, MD | Email: wayne.altman@tufts.edu |
| 11 Water St. Arlington, MA | Tuesday evenings from 6-9pm |
During this elective you will join Dr. Wayne Altman and Dietitian Kerri Hawkins for two 90-minute Wellness Group Visit sessions. You will learn about caring for patients in the group setting.
| Palliative Care | |
| Bethany-Rose Daubman, MD | Email: Bethany-Rose_Daubman@dfci.harvard.edu |
| Massachusetts General Hospital (MGH) |
Palliative care is a multidisciplinary approach to care of patients with serious illness, providing symptom management, elucidation of goals of care, and a focus on quality of life. During this elective experience, students will have the opportunity to shadow Dr. Bethany-Rose Daubman, a family physician who provides palliative care to patients at Massachusetts General Hospital (through inpatient consultations as well as care of patients admitted to the Inpatient Hospice Service at the end of life).
| Dermatology Procedures | |
| Bonnie Engelbart, MD | Email: bengelbart@challiance.org |
| Tuesday afternoons |
Spend a half day assisting in a Family Medicine Dermatology procedures clinic. Patients are referred from other primary care physicians at Cambridge Health Alliance.
| Urgent Care |
Lahey Health Urgent Care |
| Miguel Martinez, MD | Email: miguel.a.martinez@lahey.org |
| 305 Gloucester Crossing Rd, Gloucester | Contact Dr Martinez to set up time |
During this elective you will spend a half a day with Dr. Martinez, medical director of Lahey Urgent Care, in the Gloucester Center, 305 Gloucester Crossing Rd. You will learn to diagnose and manage minor acute illness and trauma. Skilled labs on reading x-rays, suturing and splinting will also be offered. Clinic times will be on Monday or Friday.
Students can contact me directly via email to set up the elective. No special badges required, but please dress professionally and wear white coat with school ID.
| Serving the Underserved – Sharewood | |
| Sharewood | Email: administrator@sharewood.info |
| The First Church in Malden | Tuesdays 6:30pm – 9pm |
| 184 Pleasant Street, Malden 02148 |
Sharewood is a free health clinic run by Tufts medical students. Sharewood offers care to the medically underserved populations of greater Boston. Sharewood provides free clinical, case management, and laboratory screening services (psychiatric, dental, and ophthalmic services are sometimes available). As a third-year student, you will independently see patients at Sharewood and precept them with the attending physician. You will also teach first and second years.
| Suboxone Group Visits | |
| Randi Sokol, MD | rsokol@challiance.org |
| 195 Canal Street | Thursday afternoons |
| Malden, MA 02148 |
Students will rotate through a “Suboxone Group visit” observing 9-16 patients who struggle with opioid use disorder and alcohol use disorder (on either bupreonorphine or IM naltrexone for medication maintenance) participate in a shared medical appointment (SMA). During the SMA, patients “check in” about their week and engage in a psychotherapeutic modality related to their addiction (12-step reading, practicing healthy coping mechanisms, relapse prevention, motivational interviewing, and other fun and engaging activities!) There are two one-hour long back to back groups followed by a one-hour interdisciplinary team meeting, in which the FM Attending, resident, addictions nurse, front desk staff member, and medical assistant discuss patient care.
| Transgender Care | |
| Deb Bershel | dbershel@gmail.com |
| 260 Elm Street, #105 | Davis Square Family Practice |
| Somerville, MA02144 |
Spend a half-day or full day with Dr. Deb Bershel, a family physician who specializes in transgender care. Her office in Davis Square focuses on personal health and wellbeing, even if it does not fit in with traditional Western medicine. Her clinical practice has a concentration in transgender health care as well as neurofeedback and low laser therapy. Dr. Bershel is an active member of WPATH (World Professional Association for Transgender Health).
Greater Springfield Options
| Addiction Medicine | |
| Peter Kassis, MD | 413-584-2173 |
| Email: pkassis@cleanslatecenter.onmicrosoft.com |
Experience care for patients with addiction with a family physician at the CleanSlate Center
| Urgent Care | |
| Louis Strauss, MD | Louis.StraussMD@baystatehealth.org |
| 325B King Street | |
| Northampton, MA | 10am-8pm M-F; 9am-5pm Sat/Sun |
Urgent care is a walk-in clinic focused on the delivery of ambulatory care in a dedicated medical facility outside of a traditional emergency room. Urgent care primarily treats injuries or illnesses requiring immediate care, but not serious enough to require an ER visit. We commonly perform small office based procedures including laceration repair, splinting, abscess I+Ds, and joint injections.
| Supportive and Palliative Care | |
| Division Hematology/Oncology | |
| Lucinda Cassells, MD | Lucinda.Cassells@bhs.org |
| Baystate Regional Cancer Program | 413-794-9338 |
| 3350 Main Street, Springfield, MA | Tuesdays; Wednesday mornings |
Spend a half day in the Supportive Care Clinic at the D’Amour Center for Cancer Care which is the outpatient clinical hub of the Baystate Regional Cancer Program. This clinic provides interdisciplinary assessment and management of symptoms caused by cancer and its treatment. Our patient population spans the cancer care continuum: patients receiving aggressive treatment with intent to cure, survivors, patients with relapsed/advanced cancer receiving treatments with palliative intent, and patients approaching end of life.
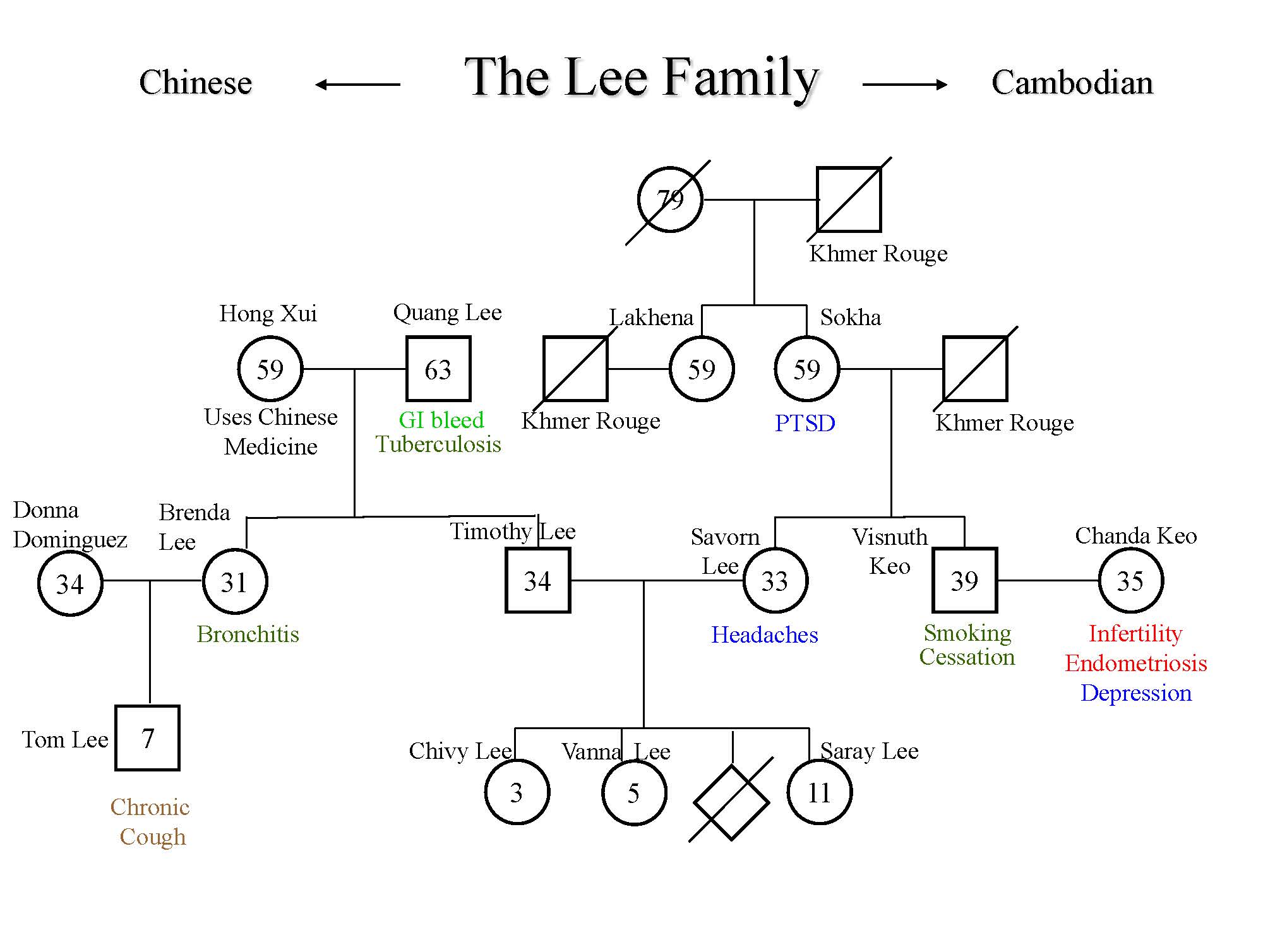
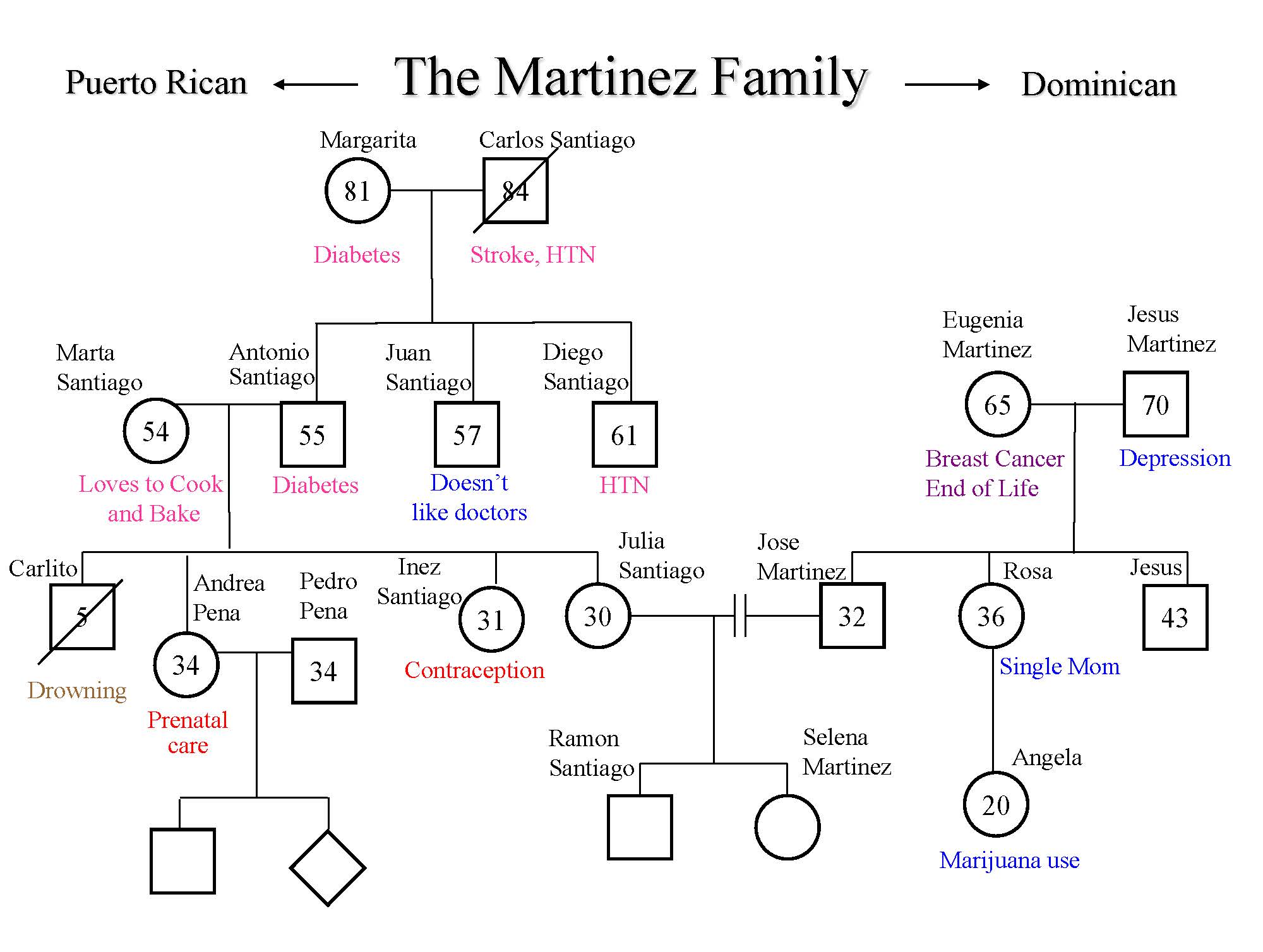
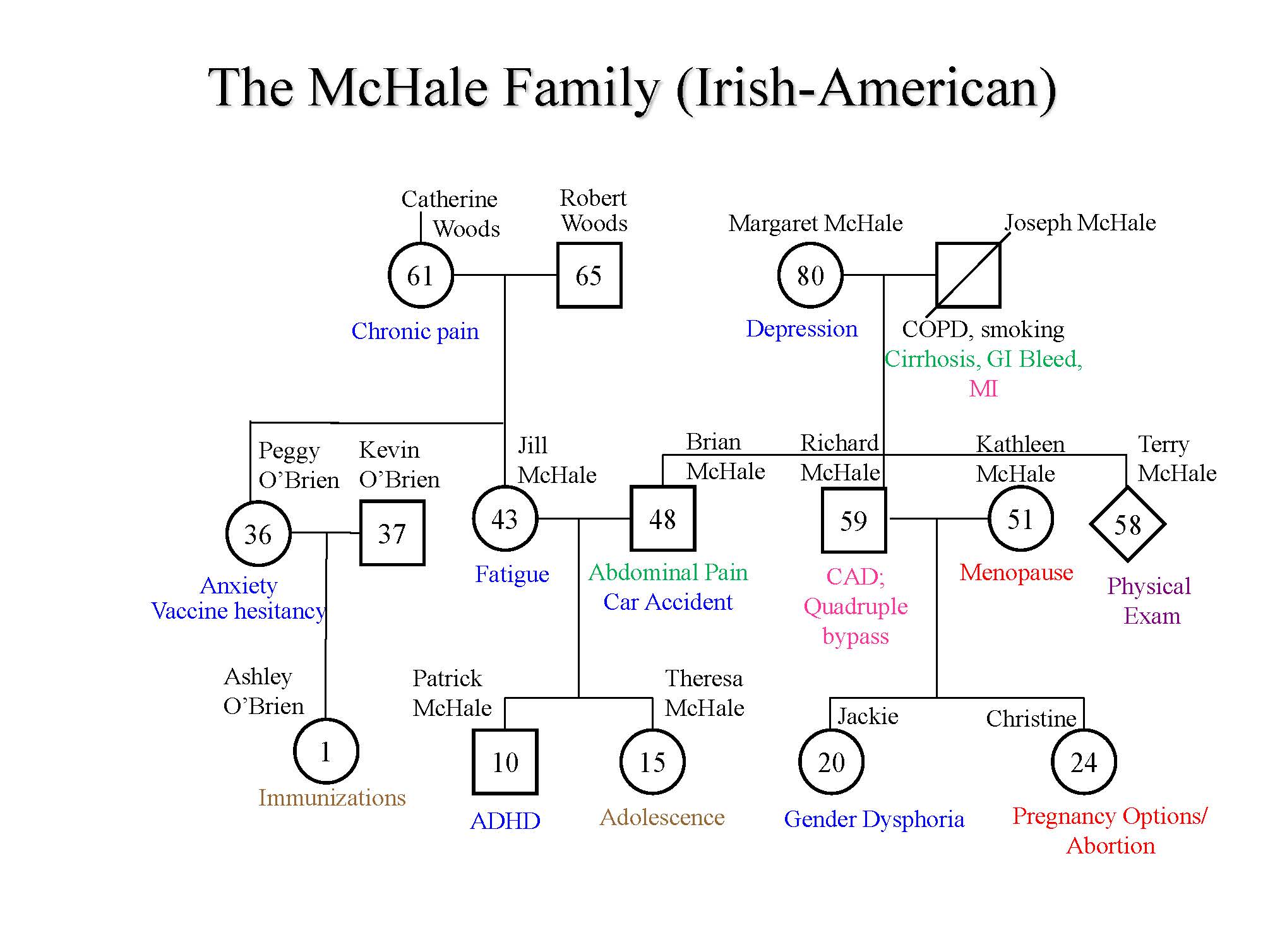
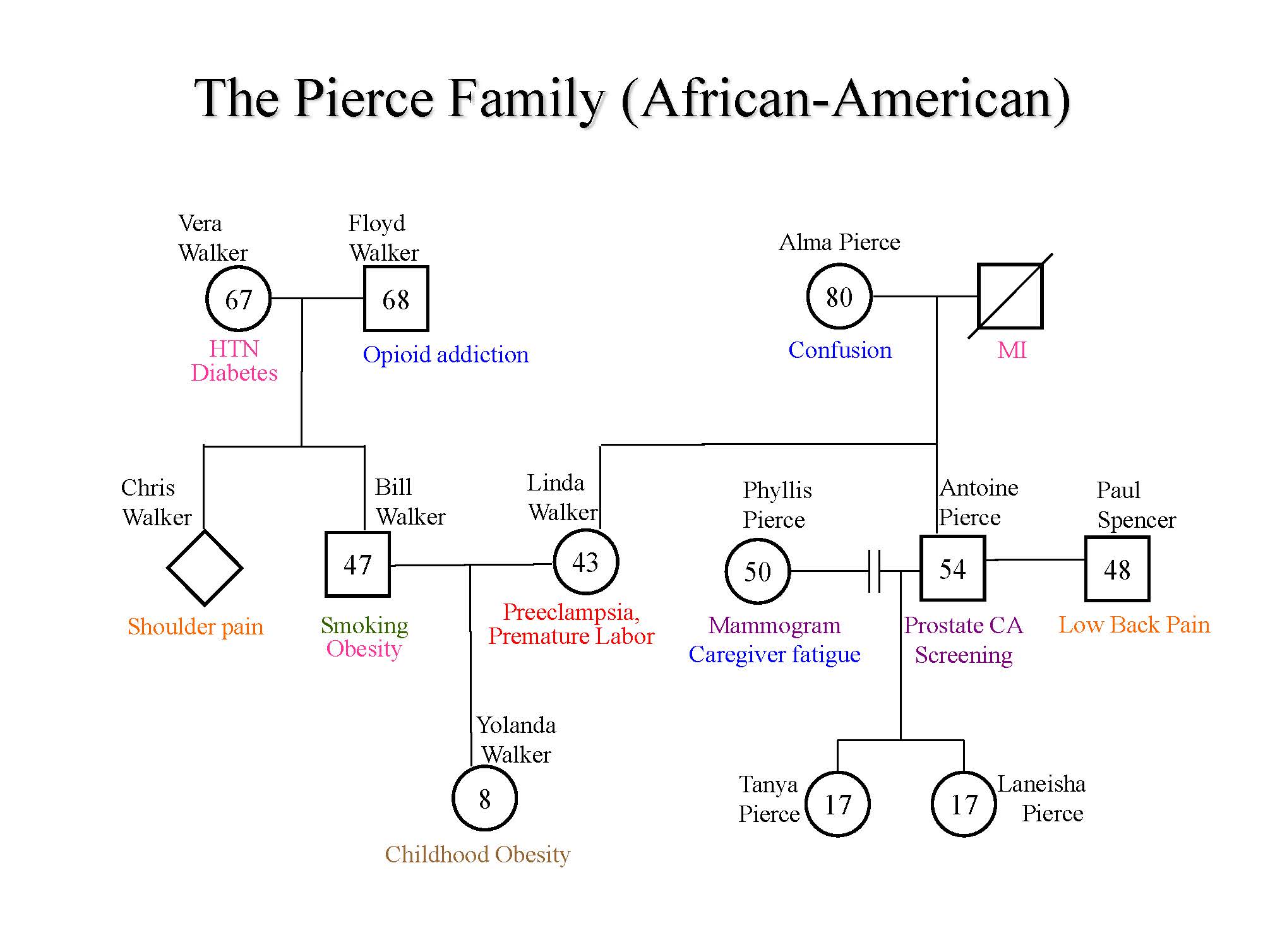
Genograms