Other Resources (Not On Exam)
Global Health and Obstetrics
Reading: Shoulder Dystocia and the HELPERR Mnemonic
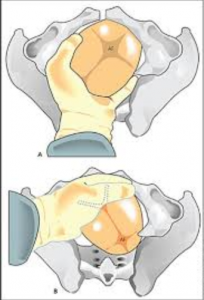
Manual Rotation of the OP Fetus
- Can confirm with U/S
- Fully dilated
- Counsel pt regarding discomfort – if available can bolus epidural
- Middle finger to base of occiput
- Cupped hand over crown
- Flex head c contraction while simultaneously rotating the shortest way to OA
- Can have assistant milk the shoulder over
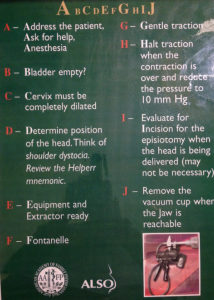
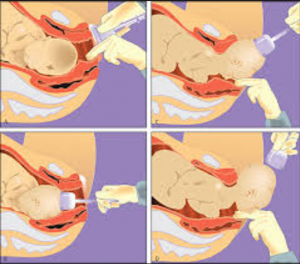
Vacuum Assisted Vaginal Delivery
- Must be +2 station
- Follow ABCD mnemonic
- Pull with contractions
- Reduce suction between contractions
- Halt if:
– 3 pop offs
– No progress with 3 consecutive pulls
– No more than 20 minutes
Correct Cup Placement
Minimize cephalohematoma and subgaleal bleeds
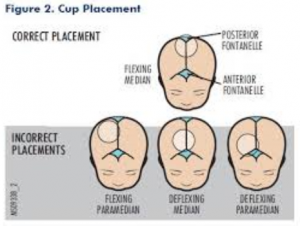
Cup Replacement and Removal
When placing, ensure that vacuum is free of any vaginal tissue
Remove cup when jaw is reachable
1st TRIMESTER MISCARRIAGE MANAGEMENT IN LOW-RESOURCE REGIONS
INTRODUCTION:
- 67,000 women die of complications from inadequately-treated abortions (spontaneous and induced), making up 13% of all pregnancy-related deaths (1)
- Developing countries are more likely to have anti-abortion laws, causing increased amount of unsterile abortions by clinicians with insufficient training. These procedures have high risk of incomplete abortions, hemorrhage, and infection.
- Curettage of the uterus in miscarriage management is associated with decreased risk of hemorrhage and retained tissue, but is associated with increased infection rate compared to presence of retained tissue. (7)
- In low-resource settings, management with Manual Vacuum Aspiration is not always sustainable due to time-consuming training or unavailability of equipment. D&C has been practiced instead, which has been associated with a higher rate of complications & infections. (3)
MANAGEMENT OPTIONS
MISOPROSTOL: effective in 79% of women with miscarriage (all types) by 7 days
- Misoprostol medical management of both incomplete miscarriage and early fetal demise has been shown to be an effective and inexpensive method of evacuating the uterus contents when compared to expectant management and surgical evacuation.
- Dosing: No studies comparing dosing regimens.
- WHO recommendation:
- Incomplete or Inevitable 1st Trimester Pregnancy Loss: Misoprostol 800 mcg PV, repeated after 3 days if needed
- Ensure follow-up in 7 days, as ~7% will have incomplete evacuation of the uterus and will require intervention at Day 7
MANUAL VACUUM ASPIRATION: 90-99% success rate
PREPARATION:
- If Rh negative, offer 50 mcg of Rhogam. Can use 300 mcg if that is all that is available.
- Should be given at the time of the procedure, or within 72 hours to prevent isoimmunization
- One dose of Doxycycline prior to MVA has been shown to decrease infections. No data supporting use of antibiotics after MVA.
- Pre-medication with Naproxen or Ibuprofen decreases pain scores after procedure.
EQUIPMENT:
-Speculum
-Tenaculum
-22 to 27 gauge spinal needle, or a 22 to 27 gauge needle with 3-inch extender
– 0.5% or 1.0% lidocaine with epinephrine, vasopressin or 8.6% sodium bicarbonate
-Tapered cervical dilators
-Uterotonic medication (to have available for hemorrhage)
-Ring forceps
-4×4 gauze
-Cannula
-MVA ( or electronic vacuum aspirator with tubing)
HELPFUL BUT NOT NECESSARY
-Bowl for products of conception
-Mesh strainer
-Glass container to view products of conception
-Povidone-iodine solution
PROCEDURE:
1) Position woman in dorsal lithotomy position
2) Perform bimanual examination to verify size and position of the uterus
3) Place speculum to visualize the cervix
4) OPTIONAL: Prepare the cervix with iodine or chlorhexidine. Studies do not show benefit to prevent infections with this step, but also no harm has been show if this step is used.
5) Place Tenaculum:
Place the tenaculum on the anterior cervical lip, unless the uterus is retroflexed, in which case it has been shown to be beneficial to place the tenaculum on the posterior cervical lip. OPTIONAL: The use of lidocaine anesthesia of the cervix prior to tenaculum placement.
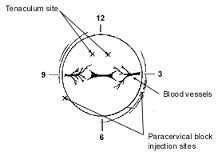
6) Paracervical Block:
- Inject 10 cc lidocaine at 4:00 and 8:00 on the cervical clock, at the reflection of the cervix from the vaginal mucosa. Inject as inserting and withdrawing the needle. Injections including deeper injections of lidocaine into uterine muscle have shown improved anesthetic outcomes.
7) Cervical dilation:
- No need to sound the uterus prior to dilating.
- Use tenaculum to straighten out the cervical canal/uterus.
- Start with a 5mm dilator and insert in the cervix, holding the dilator like a pencil in the center
- If cervix appears to be tight, hold dilator in the cervix for 20 seconds prior to removing. If easy passage, can remove immediately.
- Continue dilating with next size dilator in the same fashion until dilated to desired size. Dilate to the millimeter of the number of weeks estimated gestational age (i.e. If 7 weeks EGA, dilate to 7 mm cervical os opening).
- Routine cervical ripening is recommended by WHO for:
- Adolescents < 18 years old
- All pregnancies of EGA > 12 weeks
- Nulliparous women > 9 weeks
- Difficulties inserting dilators
in hopes of decreasing perforation in these high risk populations.
- Misoprostol 400 mcg is the recommended dose. Can be given 2 hours prior to procedure sublingually, or 3-4 hours prior to the procedure vaginally for best results.
- Osmotic cervical ripening with laminaria is also an option.

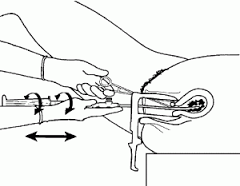
8) Aspiration:
- Create suction by closing the valves and pulling back on the plunger.
- Attach the sterile cannula.
- Insert the sterile cannula into the dilated cervix and into the uterus until the resistance of the fundus is felt.
- Open the valves to create suction and use a twirling and back-and-forth motion to aspirate the contents of the uterus. Aspiration should continue until the uterus has a gritty sensation and no additional tissue is passing through the cannula.
- You may need to empty the cylinder of the products of conception and continue with multiple passes, as the cylinder loses suction as it fills.

9) Evaluate the Products of Conception:
-Products of conception are best visualized with blood and mucous washed away through a mesh strainer. The products can then be placed in a clear glass dish with water and are best visualized with a backlight behind the glass.
10) Remove the tenaculum. Remove blood from the vaginal vault with cotton swabs or 4×4 gauze on a ringed forceps. Observe for bleeding.
11) Remove speculum and observe for bleeding for 15 minutes.
COMPLICATIONS AND MANAGMENT
- Difficult to place cannula: Can use a sterile sound and place the cannula over the sound.
- If no tissue passes through the cannula, the cannula may be clogged. Move around the cannula in the uterine cavity or remove the cannula completely and reinsert.
- Overdilation of the cervix can cause loss of suction and inability to aspirate contents. If this occurs, a larger cannula may need to be used.
- Post-procedure hemorrhage: Risk factors include advanced-maternal age, increased parity, history of obstetric hemorrhage, fibroids, history of uterine scar
- 2 large-bore IVs
- Assess for cervical laceration
- Bimanual massage
- Uterotonics (Oxytocin 10-20 units, Ergonovine 0.2mg, buccal or oral Misoprosol 400 mcg)
- Ultrasound for retained POCs
GLOBAL HEALTH WORK: What to ask before you go
Finances:
How much money do you need? What if you plan to travel back home? What if someone gets sick and you need to return urgently?
Work environment:
Organization: What is the structure of the facility? Is it run by local leaders or international doctors? What is the relationship of the foreign physicians with local physicians, leaders and workers? What is the relationship between the organization and the community it serves? How do your skills fit with the needs of the community and the organization?
Scope of practice: What things will you have or not? Blood transfusions? Antibiotics? Access to OR? What is the specialist referral structure?
Personal Safety:
What is the personal risk of infection, violence, hunger?
What health insurance should you get? Will it cover transport back home for medical causes?
Travel with family:
Will you bring children? Where will they go to school? How about your partner? What will your partner do there?
Motivations:
Why do you want to go? What if you get there and you don’t feel like you’re helping as much as you thought.
Strategies:
Talk, talk, talk. Ask anyone who’s had similar experience how it’s been. Definitely ask to speak to other physicians who have worked in the organization.
Self Care
Think about what you will do when –
– You’ve worked too many hours and you feel alienated from your work
– You feel under appreciated by your patients or local colleagues
– That one thing about the place you live that bugs you becomes overwhelmingly annoying
– Someone you love is sick or dies at home
– You have a bad outcome with a patient and their family blames you or the facility you’re working in
– You question the ethics of how you are practicing medicine
Strategies:
– Do frequent check ins with yourself to address how you are feeling.
– At some point you will think “what is wrong with these people?!”It’s OK! Just make sure to get over it quickly.
– Have a fellow foreigner who can help you through hard times.
– Have local friends so you feel community even if you are far away from yours.
– Be flexible to a point, but set boundaries. Know what you will and will not do at work and in your scope of practice.
Resources:
Articles:
Sheather, J. and Shah, T. “Ethical Dilemmas in Medical Humanitarian Practice: Cases for reflection from Médicins Sans Frontières.” J Med Ethics. 2011;37:162e165.
Hottinger, D. “An Ethic for Working in Haiti.” Minnesota Medicine. August 2013.
Singer, P. “Beyond Helsinki: A Vision for Global Health Ethics.” BMJ 2001; 322
(For a very negative view on global health) Illich, I. “To Hell with Good Intentions.” Speech delivered at the Conference on InterAmerican Student Projects (CIASP). Cuernavaca, Mexico. April 20, 1968
Organizations:
Peace Corp: Global Health Service Partnership
Mission Doctors (Catholic Organization, but connections with hospitals all over the globe)
Idealist.org: Lots of organizations advertise for international volunteers here. Definitely look well before you leap!
Health Insurance:
1st step is to see what your insurance covers, if you have any. Some partially cover transportation (even airlifts) back to the US.
Additionally – all the major American health insurance companies (Cigna, Aetna, Blue Cross Blue Shield have international packages)
Funding:
Benjamin H Joseph, MD Fund – A good resources for medical students and residents
Global Health Toolkit:
Practical Resources for Docs Doing OB and Other Medical Care in Low Resources Settings
SMARTPHONE APPS
GENERAL MEDICAL APPS (ideally these point of care apps can work offline)
- General: Epocrates / Medscape / Micromedex / Medcalc / AAFP-AFP
- EBM: Dynamed / Uptodate / Essential Evidence Plus / Journal Club (summary of landmark mostly non-OB trials)
- Emergency: Urgent Care (Marc Brancel), OrthoTrauma (Marc Brancel), Ortho Traumapedia, Fast facts for trauma care, ATLS 2014, Critical Care ACLS Guide
- Josh Steinberg apps: pap guide, warfarin guide, ABG eval, preop eval, pneumonia guide, PE and DVT tool, Rabies
- PD: Kid norm / Growth charts / Paediatric Emergencies
- Anesthesia: Stat intubation, Anesthesia Drugs: Fast!, Anesthesia drips, Critical Care ACLS Guide
- Other: Sanford’s, Insulin DM2, Eponyms, iGeriatrics, Physical Exam, Shots by STFM
OB APPS
- OB +Newborn (Marc Brancel), OB wheel,, EFM Guide (Steinberg), Apgar, BiliCalc , Lactmed, Neotube, Bishop score, GBS guide, Breastfeeding management, FHR 5-Tier
GENERAL INTERNATIONAL TRAVEL APPS
- Convert (converts weights, lengths,etc), Language dictionary, Google translate, Skype, Talkatone, TripIt, DocScanner (makes photos into PDFs), Kayak, Tripadvisor
PERSONAL APPS
- Dropbox, Postagram / Ink Cards (to send postcard back home $1-2), NPR, Audible (books), Stitcher, Pandora, Spotify, MLB.com (to follow the Red Sox from anywhere in the world), Netflix, ‘Stache Bash
WEBSITE BASED RESOURCES
- General: Uptodate, Dynamed, Essential Evidence Plus, AFP
- Medbox.org – free online source of Global Health Toolkits, Guidelines, Resources, etc (good for browsing). Has downloadable textbooks, videos, WHO documents, etc. Wealth of free information
- Medline: Through your university or HINARI [Free library resource for unaffiliated resource poor areas]
- Perinatology.com: policies, procedures and protocols – lots of helpful links
- UNC OB Practice Guidelines: OB Practice Guide, simply written, referenced, peer-reviewed –
- Neonatology Online Handbook: such as peer-reviewed sites with housestaff NICU Manuals, i.e. USCF, U of Iowa
- Medical Aid Films: simple videos for health education http://medicalaidfilms.org/
- Ultrasound basics: Ultrasoundpaedia.com
- Breech vaginal delivery video: https://www.youtube.com/watch?v=_UzvOwF9C78
MEDICAL BOOKS
- An OB pocket book (light, fairly comprehensive, management based)
- Obstetrics, Gynecology and Infertility: Handbook for Clinicians (Gordan 2007)
- Comprehensive Handbook: Obstetrics & Gynecology (Zheng 2009)
- Tarascon OB/Gyn Pocketbook, (Callahan, 2014)
- ALSO Course Binder / Resources
- Integrated Management of Pregnancy and Childbirth [IMPAC]. A guide for midwives and doctors.
- WHO District Hospital Surgical Manual Series: Free / translated into French, Korean, Farsi, Mongolian, etc
- General Surgery (WHO, 2003), OB/Gyn, Ortho and Trauma (WHO, 1991), Anaesthesia (WHO, 2000)
- The “King Series”: Primary Surgery: Volume 1: Non-Trauma / Volume 2: Trauma / Primary Anaesthesia
- King M, ed. Oxford Press; 1990. [640 pp] / 1987. [387 pp.] / 1986. [169 pp]
- The majority of the Tarascon Series; i.e. Hospital Medicine, ICU, Primary Care
- Basic Guide to Anesthesia for Developing Countries, Volumes I/II, Daniel Moos (available on Medbox.com)
- Ultrasound book: Introduction to bedside ultrasound, Vol I+II, Mike Mallin, Matthew Dawson(E-books)
- A Derm book: Habif or Fitzpatricks
- A Procedures book: Procedures; Pfenniger, 2003 or Tarascons Medical Procedures Pocketbook; Esherick, 2012.
TEACHING RESOURCES (for OB Care)
- Cervical dilation model
- Family Centered Maternity Care Course slides
- Papaya with MVA – see ipas.org
- Consider a pelvic model if teaching will be a focus
POINT OF CARE RESOURCES (for OB Care)
- A good headlamp
- urine dips
- blood pressure cuffs
- Stethoscopes
- Hand held dopplers
- nitrazine paper
- KOH
- microsope slides / cover slips
- sterile packets of lube
- containers of lube for the U/S machine
- measuring tape
- Gloves
- a speculum with a light source (if no good lamps)
- MVA with dilators and cannulas (see ipas.org)
- syringe with needle extender
- Vacuums
- Meds:
- nifedipine PO is easy, miso, terb, pitocin, magSO4, methergine, hemabate
- spinal kits
- portable U/S
- Biliwand
- FOBT cards and developer
- EFM
- paper for EM
- Bakri balloon
- red rubber catheters
- Foley bulb or Cook double balloon catheter
- Suture
- laminaria
- local anesthetic
- right angle retractors (for cervical lacs)
RECOMMENDED READING FOR THOSE INTERESTED IN GLOBAL HEALTH:
BOOKS
- Albert Schweitzer, a biography: Professor George Marshall and David Poling
- Pathologies of Power. Paul Farmer
- Cutting for Stone: Abraham Verghese
- I, Rigoberta : Rigoberta Menchu
ARTICLES
- Hottinger, D. “An Ethic for Working in Haiti.” Minnesota Medicine. August 2013.
- Illich, I. “To Hell with Good Intentions.” Speech delivered at the Conference onInterAmerican Student Projects (CIASP). Cuernavaca, Mexico. April 20, 1968. (For a very negative view on global health)
- Marmot, M, “Health in an Unequal World” Lancet 2006; 368; 2081-94
- Nolan, A, “Four stages of spiritual growth in helping the poor” http://www.catholiccincinnati.org/wp-content/uploads/2011/02/FourStages_SpiritualGrowth_by_Nolan.pdf
- Sheather, J. and Shah, T. “Ethical Dilemmas in Medical Humanitarian Practice: Cases for reflection from Médicins Sans Frontières.” J Med Ethics. 2011;37:162e
- Singer, P. “Beyond Helsinki: A Vision for Global Health Ethics.” BMJ2001; 322
“I slept and dreamt that life was joy.
I awoke and saw that life was service.
I acted and behold, service was joy.”
-Rabindranath Tagore
Created by Andrew Smith, MD
