4 Didactic Day 4
DD4
Introduction to Underserved Medicine
Learning Objectives
- Define and list examples of social determinants of health
- Describe the role of community health centers
SOCIAL DETERMINANTS OF HEALTH (SDH):
- Economic and social conditions that result in differences in health status apart from genetic and individual biologic factors
- o WHO defines SDH in the following way:
- “The poor health of the poor, the social gradient in health within countries, and the marked health inequities between countries are caused by the unequal distribution of power, income, goods and services, globally and nationally, the consequent unfairness in the immediate, visible circumstances of people’s lives – their access to health care, schools, and education, their conditions of work and leisure, their homes, communities, towns or cities – and their chances of leading a flourishing life. This unequal distribution of health-damaging experiences is not in any sense a ‘natural’ phenomenon…Together, the structural determinants and conditions of daily life constitute the social determinants of health.” (WHO Commission on SDH, 2008)
- o The Robert Wood Johnson Foundation (RWJF) has identified a simpler phrasing to describe SDH:
- “Health starts where we live, learn, work and play.”
- o WHO defines SDH in the following way:

SOCIAL GRADIENT OF HEALTH
- Life expectancy is shorter and disease is more common further down the social / socioeconomic ladder
WHAT ARE SOME EXAMPLES OF SOCIAL DETERMINANTS OF HEALTH?
- Education, employment opportunities, water, sanitation, housing, food access, level of social inclusion / exclusion, social support networks, stress, early childhood development, race/gender/sexual orientation/etc (as they impact the other SDHs)
WHAT IS THE RELATIVE IMPACT OF SDH ON HEALTH VARIANCE / OUTCOMES? A lot; probably more than half
- Various researchers have shown that health care accounts for only 10-25% of the variance of health over time.
- The rest is shaped by genetics (up to 30%), health behaviors (30-40%), social and economic factors (15-40%) and physical environmental factors (5-10%)
- SDH effectively create remarkably disparate health outcomes, even within the same city, county, state and country. For example:
- o Life expectancy differences-metro Washington D.C.: 72 (City Center)
- o Life expectancy differences in the U.S. 66.6 (Bennett County, SD)
EXAMPLES OF SOLUTIONS
- The case studies in the WHO site http://www.who.int/sdhconference/resources/case_studies/en/ present successful examples of policy action aiming to reduce health inequities, covering a wide range of issues, including conditional cash transfers, gender-based violence, tuberculosis programs and maternal and child health.
CENTRAL FIGURES IN WORK ON SDH:
- Michael Marmot: (1945-present) British epidemiologist and international statesman on health inequities who was a lead investigator in the Whitehall Studies of British civil servants (assessing health inequities in Great Britain) was the founding chair of the WHO Commission on Social Determinants (2005-2008); Lecturer / author of “Health in an unequal world” (Lancet, 2006; 368: 2081-94)
- Paul Farmer: (1959-present) American anthropologist and physician best known for his humanitarian work providing health care to rural and under-resourced areas in developing countries, beginning in Haiti. Co-founder of the international social justice and health organization, Partners In Health (PIH), and professor at Harvard Medical School. Author of numerous books and publications, including Pathologies of Power.
- Rudolf Ludwig Carl Virchow: 19th century Germany doctor, anthropologist, pathologist, prehistorian, biologist, writer, editor, and politician. Ahead of his time in pushing early advances in public health. Considered by many to be the founder of social medicine. Since disease so often results from poverty, he said, then physicians are the “natural attorneys of the poor”, and social problems should largely be solved by them.
“We pledge to bind ourselves to one another, to embrace our lowliest, to keep company with our loneliest, to educate our illiterate, to feed our starving, to clothe our ragged, to do all good things, knowing that we are more than keepers of our brothers and sisters.
We are our brothers and sisters.”
-Maya Angelou
Optional Readings:
Pathologies of Power: Paul Farmer
Savage Inequalities: Jonathan Kozol
The End of Poverty: Jeffrey Sachs
Development as Freedom: Amartya Sen
Immigrant Medicine: Patricia Walker and Elizabeth Garnett
“Why America is Losing the Health Race”, Allan Detsky (The New Yorker, 6/11/14)
“Health in an Unequal World”, Michael Marmot (Lancet 2006; 368: 2081–94)
Created by Andrew Smith, MD
Community Health Centers: A History
Required Reading: Massachusetts League of Community Health Centers
Optional Reading: Get the Facts
Optional Reading: Community Health Centers: Leveraging the Social Determinants of Health
Addiction
Learning Objectives
- Describe a primary care approach to addiction.
Definitions:
Addiction is a primary, chronic disease of brain reward, motivation, memory, and related circuitry. Dysfunction in these circuits leads to characteristic biological, psychological, social, and spirit manifestations. This is reflected in the individual pursuing reward and/or relief by substance abuse and other behaviors. The addiction is characterized by impairment in behavioral control, craving, inability to consistently abstain, and diminished recognition of significant problems with one’s behaviors and interpersonal relationships. Like other chronic diseases, addiction can involve cycles of relapse and remission. Without treatment or engagement in recovery activities, addiction is progressive and can result in disability or premature death.
(American Society of Addiction Medicine)
Opioids vs Opiates: although often used interchangeably, opiates is officially a more restrictive term, referring only those compounds derived from the natural poppy (morphine, codeine, heroin). Opioids include those opiates, in addition to the semi-synthetic and the synthetic compounds. Practical application: a routine urine drug screen (DSU 9 means it’s checking for 9 compounds) detects opiates well but has very poor negative predictive value for semi-synthetics (hydrodone/vicodin, oxycodone/percocet, hydromorphone, oxymorphone, buprenorphine/suboxone), or full synthetics (dilaudid/fetanyl, methadone, tramadol/ultram).
Dependence means that there is a physiologic requirement for the substance. A lack of this substance induces withdrawal. Dependence is a physiologically normal reaction to taking certain medication frequent enough to constantly have the substance in circulation (not only controlled medications: SSRIs, caffeine, beta blockers, etc.)
Tolerance means that increasing doses of a medication are needed to achieve the same effect. Tolerance is reversible, with the rate depending on the pharmacokinectics of the particular drug, as well as dosage and frequency of use.
Abuse is use of a substance out of socio-culturally accepted norms. There is no accepted use of heroin, so it is always an abuse. Alcohol, on the other hand, can either be used or abused.
Addiction (see above): loss of control, continued use despite negative consequences, compulsion to use.
Numbers:
- SAMHSA 2007: 1 out of every 200 in US will try illicit drugs any year, 23% will become dependent. Every year, 1 of 800 in US becomes addicted.
- Annually, addiction costs over $500 billion: work loss due to health, illness for users and victims, costs of medical treatment, cost to the justice system, to infrastructure.
- #1 abused substance category: prescribed medication (overtook marijuana 3 years ago, in all categories)
- #1 abused medication in the US: vicodin
- Substance abuse ranks among the top 10 health problems in the United States (NIH 2000)
- In Massachusetts, addiction claims 2 deaths per day.
- In 2007, the Merrimack Valley (Lawrence, Lowell, Haverhill, etc…) was ranked as the number 1 heorin dealing area in the country
Suboxone (buprenorphine) vs Methadone
- Both valuable treatment options
- Methadone, for addiction treatment, can only be given in methadone clinics (inpatient stay also if approved by clinic), daily dose, random testing, no ceiling, commonly measured in UDS, large pain control potential.
- Buprenorphine: can be prescribed by any certified physician (8 hour training course), can be prescribed monthly, needs specialized urine test, blocks all other opioids, medium pain control, has ceiling, little or no euphoria, risk of respiratory depression only if taken with alcohol, benzodiazepine, or sedatives.
Required Reading: A Primary Care Approach to Substance Misuse
Money and Medicine
“A wise man should have money in his head, but not in his heart.” –Jonathan Swift
“Making money isn’t hard in itself… What’s hard it to earn it doing something worth devoting one’s life to” — Carlos Ruiz Zafon
“Money is better than poverty, if only for financial reasons.” — Woody Allen
“Money can’t buy happiness, but neither can poverty.” — Leo Rosten
Reflection piece:
For the love of money, Sam Polk, NY times, Sunday review
Kiame’s Top Ten Tips for increasing the chances you’ll be happy in residency
- When post-call, never talk about anything serious with your significant other. This is a challenge because after two days and one night without you, your partner will have stacked up crucial issues to resolve. Be polite, honest and firm: “I apologize: call was physically and emotionally traumatic. I promise to talk about it on….”. Of course, it’s bad form to then spend 3 hours on COD or Netflix (unless it’s with your partner).
- Institute your own personal “Code pink”. Unless your hands are actually inside someone’s chest and it’s only your massaging keeping the patient alive, answer your significant other’s calls/texts/future communication system immediately. They know how busy you are (you yammer about it self-importantly at home all the time): they are not calling frivolously. My wife and I had a system: if one called the other twice in a row within a minute, it meant it the caller deemed it an emergency.
- Always use the stairs. Even if your hospital has ten floors. My residency hospital had five floors: I once calculated that using the stairs prevented me from gaining one lb a year. Not much? Think how much you’d like to be weighing 3 to 5 lbs less right now, with no effort.
- Never talk politics with anyone who is hierarchically superior to you.
- Pig out as much as you want at any meal eaten in the hospital. Once you push away from the table though, you are not allowed to eat ANY food in the hospital that you did not bring from home. No Halloween candy, no Christmas cookies, no Thanksgiving snacks, nada.
- Use the opportunity of a residency to find out what you love doing professionally. Then set up your career in pursuits of that passion.
- Marry rich.
- Never comfort someone who is not your significant other in a room that has a bed. Especially after a hard night of call. My version of this became no hugging at work. Or after work. Or ever.
- Listen carefully, smile a lot, say please and thank you, pretend to be humble.
- When post-call, never talk about anything serious with your significant other.
Created by Kiame Mahaniah, MD
HIV
Learning Objectives
- Identify indications for PrEP therapy
Required Reading: Pre-exposure Prophylaxis (PrEP) for HIV Prevention
Required Video on HIV prophylaxis
Transgender Care
Required Reading: Caring for Transgender and Gender-Diverse Persons: What Clinicians Should Know
Required Reading: Affirmative Care for Transgender and Gender Non-Conforming People
Care of the Homeless
Questions to Consider for Panel Participants at Day Break Shelter
- What situations led to you becoming homeless? Was it lack of money, lack of education, bad breaks, lack of support, divorce, drugs, abuse, loss of job, lack of affordable housing, mental health issues, a combination of things…..?
- Tell me about the risks of violence in the homeless situation. For example, risk of physical and sexual abuse, risk of robbery, risk of intimidation (being threatened by someone). How common is violence in the shelters or rooming houses(YM(W)CA)?
- While you have been or were homeless, what troubled you most about the situation? For example, fear of others, hopelessness of ever getting out, worsening medical problems, worsening addiction, lack of good food, lack of family, lack of transportation, lack of access to health care.
- Who and what services have helped you most? For example, services offered at DayBreak and The Psychological Center, friends, drug programs, medical services, bus passes, vouchers for cabs, taxi and buses, help with getting MassHealth…
- In your experience, how easy is it to get and maintain housing?
- In your experience, how are children affected?
- Do any of you have questions for all of us here i.e. health care workers in attendance today?
Required Reading: Care of the Homeless: An Overview
10 IMPORTANT ASPECTS OF CARE TO CONSIDER WHEN CARING FOR THE HOMELESS
BE RESPECTFUL: Many of our friends are victims of violence and as a result, trust levels are low, especially with the healthcare system, are low. Be respectful and in awe as to how they survive.
WITHHOLD JUDGMENT: Withhold judgment with respect to what appear to be horribly adaptive behaviors on the street with relation to drug abuse, crime …until you’ve walked a day in their shoes or at least listened to them for 6 months.
MODIFY THE GUIDELINES: Modify your guidelines and evidence-based medicine to fit the realities on the street. You wouldn’t want to give a diuretic to someone who has no access to a bathroom and who must urinate in public, a criminal offense.
CONTACT INFORMATION: Make no assumptions. Simple things such as contact info can be challenging for homeless. Instead of saying, “What’s your phone number?”, consider more sensitive questions such as “Is there a way we can get in contact with you?” or “Is there anyone who can reach you?”
FOOT CARE: For people who spend much of their day on their feet and who may not have access to clean socks on a daily basis, foot care becomes much more challenging. Whenever possible, do a good foot exam…and consider carrying around a few extra pair of socks
IDENTIFICATION AND INSURANCE: Although most homeless people are poor enough to qualify for public health insurance, the transient homeless encounter extra issues with identification and addresses. If state ID is lost or stolen it can take a long time to get back into the system and back on insurance
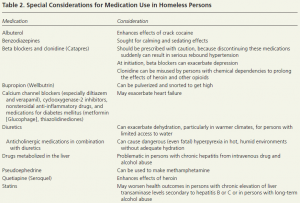
MODIFY THE MEDICATIONS YOU PRESCRIBE: Be aware of potential dangers associated with medications below (among others):
KNOW WHEN PEOPLE HAVE MONEY: Most state and federal assistance programs provide funds to people at the beginning of the month. This can create a dichotomy of experiences depending upon the time of the month. Some people will choose to stay in a hotel room or be more active in drugs at the beginning of the month when they have some cash on hand. Conversely, some may run short of food or other public entitlements by the end of the month.
GET TO KNOW YOUR PATIENT’S NARRATIVE: Get to know the individual in a laid back, open-ended manner. Try to learn about the individual’s personal narrative, including where he/she is from, how long he/she has been homeless, and what life circumstances may have led to an unstable housing situation. Show empathy and understanding, while not pushing an agenda.
MOVE AT THE PATIENT’S PACE: Client readiness is imperative to successful engagement. If a client is not ready to engage—for a host of reasons, including fear, lack of trust, or mental illness—he or she has the power to decline. Continue to show support and a consistent presence, and clients may eventually become willing to engage. Have an open dialogue with clients regarding pacing to ensure that you are working at a comfortable speed.
Sources: Vince Waite, MD – GLFHC, Cara Marshall, MD – GLFHC, Andy Smith, MD – GLFHC, Am Fam Physician. 2014;89(8):634-640, National HCH Council
