24 Embryology of the Reproductive System
EMBRYOLOGY OF THE REPRODUCTIVE SYSTEM
Learning Objectives
- To describe sexual differentiation systems from an early indifferent gonadal stage
- To describe the formation of the external genitalia
- To be familiar with common disorders of sexual development (DSD)
Lecture notes
Larsen, W.J. Human Embryology 4th Edition, Chapter 15, pp. 479-541
We also recommend that you review the tutorials on the Urogenital System developed by the University of North Carolina at:
http://www.med.unc.edu/embryo_images/unit-genital/genital_htms/genitaltoc.htm
and at the University of Indiana at:
http://www.indiana.edu/~anat550/urrepanim/index.html
Overview of Development
Genetic sex determination occurs at fertilization. The sexual genotype directs gonadal development (testes vs. ovaries), which in turn directs reproductive tract and external genitalia development. Genotypic, gonadal, and phenotypic sex assignments may be discordant.
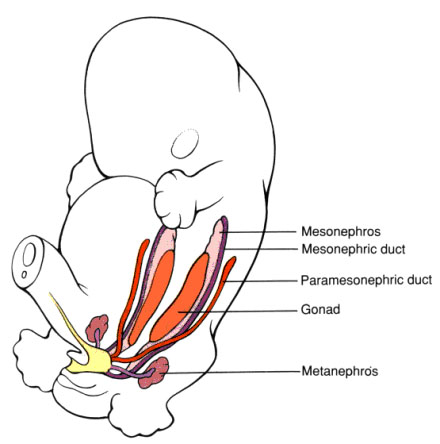
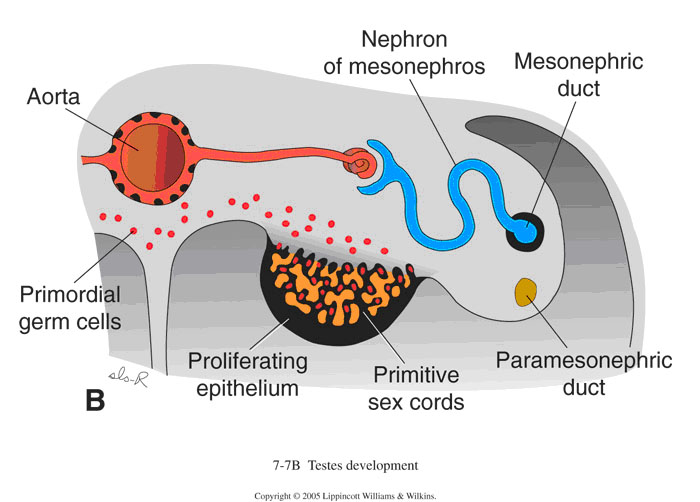
In both sexes, formation and differentiation of the gonads begins with the arrival of primordial germ cells in the intermediate mesoderm (IM). At this point we refer to it as the indifferent gonad. The germ cells migrate from the yolk sac to populate the mesenchyme of the posterior body wall at the thoracic level, and then move to the area adjacent to the developing mesonephric kidney. The coelomic epithelium responds by proliferating, thickening, and forming a pair of genital ridges.
The indifferent gonad will have both mesonephric ducts (Wolffian ducts), and paramesonephric ducts (Müllerian ducts). If development goes along the male line, mesonephric ducts remain and the paramesonephric ducts degenerate. If development goes along the female line, Müllerian ducts remain and Wolffian ducts degenerate.
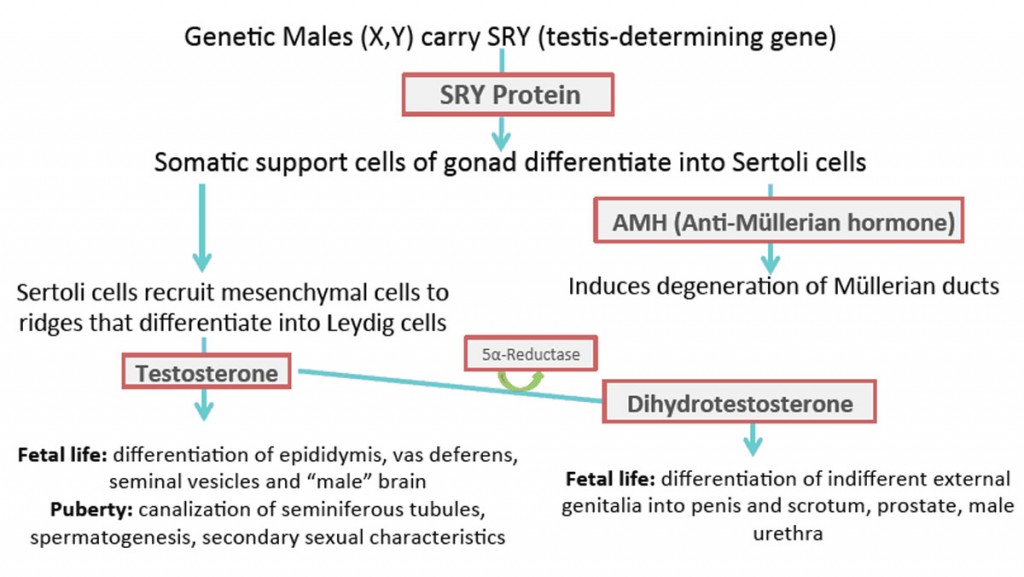
A single sex-determining factor encoded by the SRY (sex-determining region of the Y chromosome) gene controls a cascade of events leading to male development. When this transcription factor is expressed, male (46XY) development is triggered (primary sex determination). If the factor is absent or defective, female (46XX) development occurs.
Male development
- Expression of SRY protein.
- Somatic support cells begin to differentiate into Sertoli cells and envelop the germ cells.
- Sertoli cells and interstitial cells of the gonad organize to form testis cords.
- At the level of the mesonephros, where there are no germ cells, Sertoli cells organize into a set of thin-walled ducts, rete testis.
- During the 7th week, testes begin to round up and the coelomic epithelium is separated from the testis cord by a layer of connective tissue (tunica albuginea).
- Cell-to-cell contact between Sertoli and primordial germ cells within the gonadal ridge plays a key role in development of male gametes. The interaction inhibits further mitosis of germ cells.
Anti-Müllerian Hormone (AMH) and Male Genital Development
- Sertoli cells also secrete a glycoprotein hormone called AMH (Anti-Müllerian Hormone) around week 8.
- AMH causes the Müllerian ducts to regress.
- Some small ducts remain and form the appendix testis and prostatic utricle of the adult male.
- No further development of germ cells occurs until about 3 months postnatal, when germ cells differentiate into type A spermatogonia.
- The remainder of gametogenesis is delayed until puberty.
Differentiation of Testis Leydig Cells
- Week 9-10, Leydig cells differentiate and produce testosterone, which promotes survival of the mesonephric duct (necessary for development of the male reproductive tract).
- Testosterone secretion is regulated by the hormone chorionic gonadotropin, secreted by the placenta.
- After week 16, the pituitary takes over in production of testosterone.
- From testosterone, Leydig cell 5α-Reductase generates dihydrotestosterone, needed to induce male urethra, prostate, penis, and scrotum.
- Mutations affecting Leydig cell differentiation and function, or in genes involved in testosterone synthesis, generally lead to male pseudohermaphrodism.
- Leydig cells degenerate late in fetal and early postnatal life.
- At puberty, a new population of adult Leydig cells differentiates and produces androgens, which play a major role in masculinizing the brain, and initiating spermatogenesis.
Female development
- The somatic support cells do not contain a Y chromosome or the SRY gene, so they differentiate as follicle cells instead of Sertoli.
- Neither AMH nor testosterone is produced.
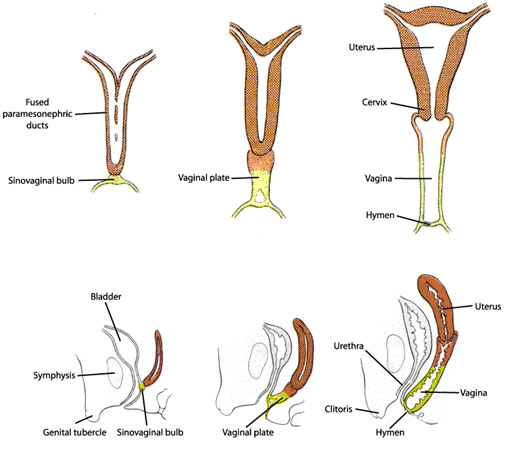
- Müllerian ducts persist and differentiate into the Fallopian tubes, uterus, and upper vagina.
- In the absence of SRY, the female gonads form primordial follicles and thecal cells (homolog of Leydig cells).
- Mesonephric ducts and mesonephric tubules rapidly disappear in females due to the lack of testosterone production.
- As soon as the fused tips of the Müllerian ducts connect with the wall of the urethra, they begin to fuse cranially, forming a short tube with a lumen, the uterovaginal canal, which becomes the uterus. The unfused cranial portions become the fallopian tubes.
- The urogenital sinus on the dorsal midline induces the formation of the sinovaginal bulb, which will eventually connect with the uterus, forming the
vagina.
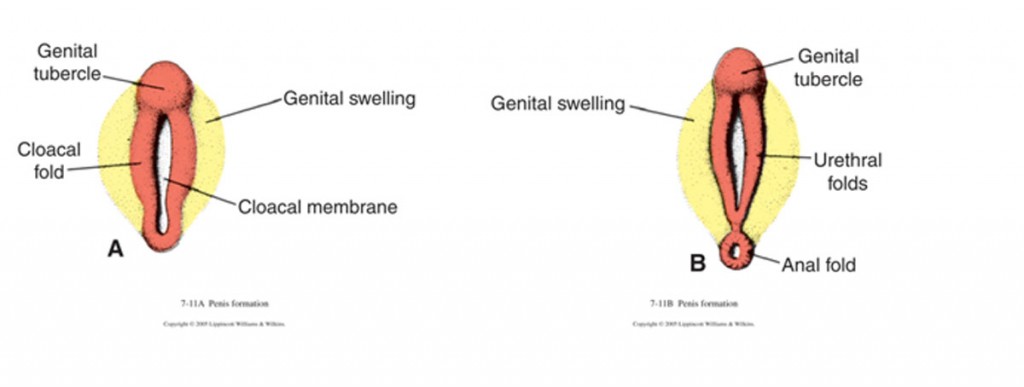
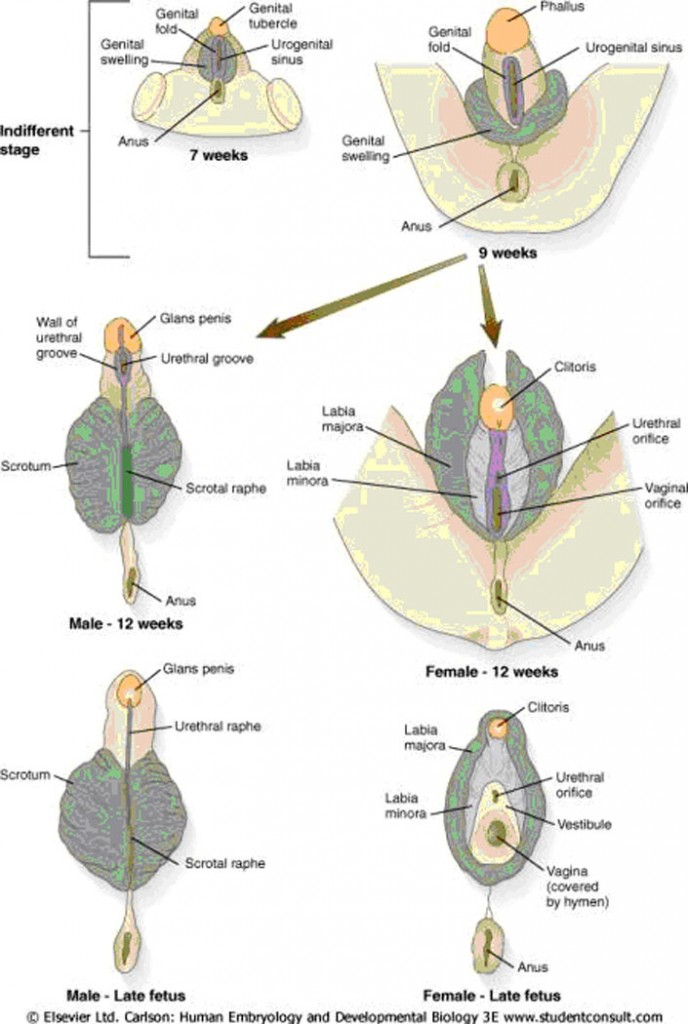
Development of the external genitalia
- Early development is similar in both sexes.
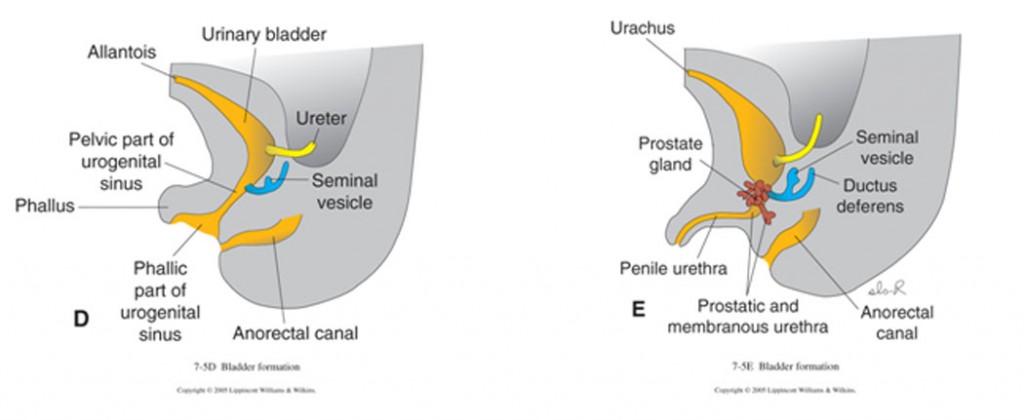
- The urorectal septum separates the urogenital sinus and anorectal canal.
- Mesoderm anterior and cranial to the phallic segment of the urogenital sinus expands, generating the genital tubercle, which eventually forms the phallus.
- Much of the floor of the phallic segment is lost, whereas the roof expands as the genital tubercle enlarges. This endodermal extension forms the urethral plate.
- Early in the 5th week the urogenital folds develop on either side of the urethral plate and meet to join the genital tubercle.
- Similarly, there is an expansion of underlying mesoderm flanking the anal membrane forming the anal folds.
- A new pair of swellings, the labioscrotal swellings, then appears on either side of the urethral folds.
- The appearance of the external genitalia is similar in both sexes through the 12th week.
- The urogenital membrane breaks down.
Male
- The endodermal urethral plate becomes excavated, forming a urethral groove along the ventral surface of the genital tubercle.
- As the phallus elongates, the urethral folds grow toward one another and fuse in the midline and extend distally toward the glans penis. This converts the urethral groove into a tubular penile urethra.
- Hypospadias result from failure of formation or fusion of the urethral folds or abnormal canalization of the urethral plate within the glans penis.
- Starting in the 4th month the perineal region separating the urogenital sinus from the anus begins to lengthen, the labioscrotal folds fuse at midline to form the scrotum, and the urethral folds fuse to enclose the penile urethra.
Female
- In the absence of an androgen, the labioscrotal swellings become the labia majora; the urethral folds do not fuse across the midline, and become the labia minora and the genital tubercle does not lengthen and becomes the glans and shaft of the clitoris.
- The sexes are visibly distinct in the 4th month.
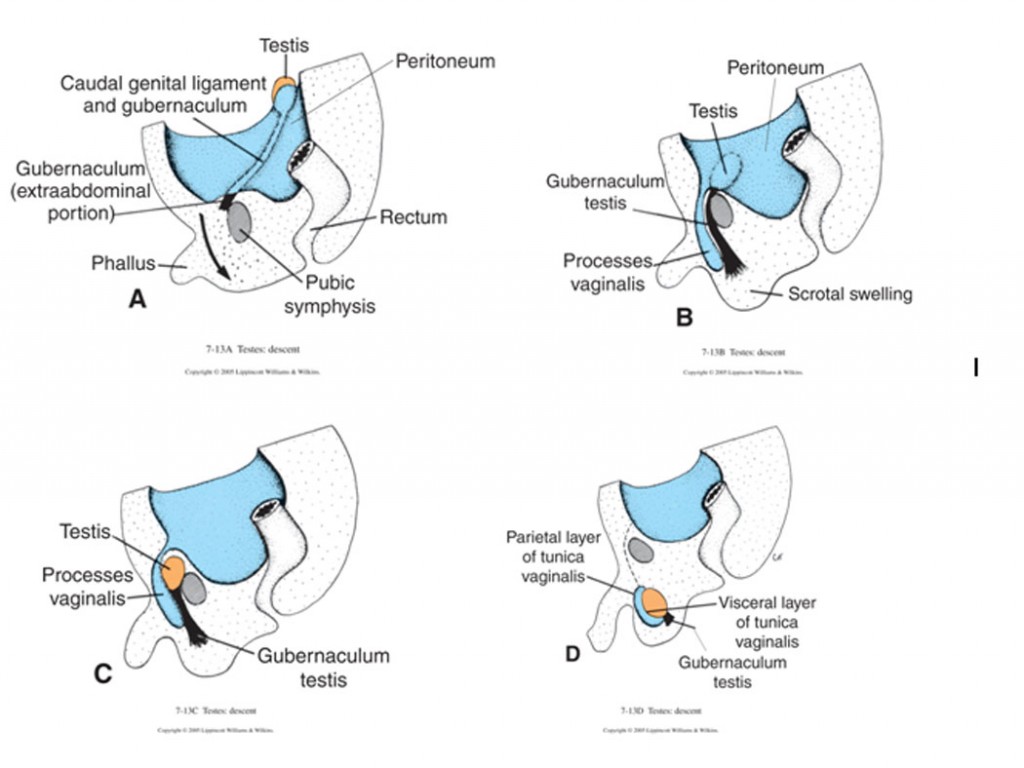
Descent of the gonads
Original position for both testes and ovaries is at 10th thoracic level. In both, the descend depend on the ligamentous gubernaculum, which condenses during the 7th week.
Male
- Between weeks 7 and 12, the extrainguinal portions of the gubernacula shorten and pull the testes down.
- Testes remain in the vicinity of deep inguinal ring from the 3rd to the 7th month but then enter the canal in response to more shortening and migration of the gubernacula.
- Within the 1st year after birth, the cranial portion of the vaginal process is obliterated, leaving a remnant sac, the tunica vaginalis, which lies ventral to the testis. During infancy, this sac wraps around most of the testis. Its lumen is normally collapsed, but under pathologic conditions, it may fill with serous secretions, forming a testicular hydrocele.
- Abnormalities in testicular descent may result in cryptorchidism (undescended testes) or ectopic testes.
Female
- The gubernaculum does not shorten but it causes the ovaries to descend during the 3rd month and to be swept out into a peritoneal fold, the broad ligament of the uterus.
- The subsequent formation of the uterovaginal canal from the caudal portions of the paramesonephric ducts also creates the broad ligaments of the uterus and pulls the ovaries into them.
- In the absence of male hormones, the female gubernaculum remains intact. The inferior part becomes the round ligament of the uterus, connecting the fascia of the labia majora to the uterus, and the superior part becomes the round ligament of the ovary, connecting the uterus to the ovary.
In both sexes, it is not rare for the entire vaginal process to remain patent, forming a connection between the abdominal cavity and the scrotal sac (indirect inguinal hernia)
CLINICAL CORRELATIONS
Hermaphrodites
True hermaphrodites are individuals that have sex chromosomes, genitalia, and/or secondary sex characteristics that are discordant or mixed. They may be chromosomal males, chromosomal females, or mosaics. It is a very rare condition.
Pseudohermaphroditism
Individuals that are born with secondary sex characteristics or a phenotype that is different from what would be expected on the basis of the gonadal tissue (ovary or testis).
- Male pseudohermaphroditism (genetic males with feminized genitals):
- Androgen insensitivity syndrome (testicular feminization syndrome) – normal-appearing female with presence of undescended testes and 46XY chromosome constitution. The external genitalia are female but the vagina ends in a blind pouch. The uterus and uterine tubes are absent
- 5α-reductase deficiency – individuals born with male gonads but usually have female primary sex characteristics. Consequently, they are often raised as girls, but usually have a male gender identity
- Female pseudohermaphroditism (genetic females with masculinized genitals)
- Results from virilizing adrenal hyperplasia, a disorder of the fetal suprarenal glands that causes excessive production of androgens
Klinefelter syndrome (males)
Presence of an extra X chromosome. Primary defect is failure of Leydig cells to produce sufficient amounts of male steroids, which results in small testes and azoospermia (lack of spermatogenesis) or oligospermia (low sperm count). Many also exhibit gynecomastia (breast swelling) and eunuchoidism (slender habitus, elongated extremities, and sparse hair).
Turner syndrome (females)
Caused by a 45X karyotype or 45X/46,XX mosaicism. Failure of normal sexual maturation at puberty, short stature and webbed neck, coarctation of the aorta, and cervical lymphatic cysts.
Anomalies of Uterus
Incomplete fusion of the lower segments of the Müllerian ducts lead to development of a duplicated uterus with or without a duplicated vagina. Failed regression of the uterine septum can lead to a bicornate uterus, a separated uterus, or atresia of the cervix. A unicornuate uterus results if one of the entire Müllerian ducts regresses or if one fails to elongate. The majority of women with Müllerian duct anomalies can usually conceive but they have higher rates of spontaneous abortion, premature delivery, and dystocia (difficult or abnormal delivery).
Defective Partitioning of Cloaca
When the urorectal septum is incomplete, fistulas form, and depending on the location of the defect there are different types:
Rectourethral fistulas – urorectal septal folds fail to grow and fuse caudally, so cloaca is not separated into urogenital sinus and anorectal canal. In males, these take the form of rectoprostatic urethral fistulas, connecting the rectum to the prostatic urethra. In females, most commonly the Müllerian ducts attach to the pelvic urethra cranial to the rectourethral fistula. The caudal undivided region of the cloaca becomes a common outlet for the urethra, the vagina, and the rectum (rectocloacal canal).
Rectovaginal fistula – when the uterovaginal canal incorporates the rectourethral fistula while migrating to a more caudal position on the posterior wall of the cloaca. In these cases, vagina and urethra open separately into the vestibule, but rectum communicates with the vagina.
Rectovesical fistula – when the entire length of the folds forming the urorectal septum fails to fuse and forms an abnormal communication between the rectum and bladder.
| Presumptive Anagen | Male Structure | Female Structure |
| Indifferent gonad | Testis | Ovary |
| Primordial germ cell | Spermatogonia | Oocytes |
| Somatic support cell | Sertoli cells | Follicle cells |
| Stromal cells | Leydig cells | Thecal cells |
| Gubernaculum | Gubernaculum testis | Round ligament of ovary and uterus |
| Mesonephric tubules | Efferent ducts of testisParadidymis | EpoophoronParoophoron |
| Mesonephric duct | Appendix of epididymisEpididymisVas deferensSeminal vesicleEjaculatory duct | Appendix vesiculosaDuct of epoophoronGartner’s duct |
| Müllerian duct | Appendix of testis | Fallopian tubesUterus |
| Urogenital sinus | Prostatic and membranous urethreaProstatic utricleProstatic glandBulbourethral glands | Membranous urethraVaginaUrethral/paraurethral glandsGrater vestibular glands |
| Genital tubercle | Glans penisCorpus cavernosumCorpus spongiosum | Glans clitorisCorpus cavernosum of clitorisBulbospongiosum of vestible |
| Urogenital folds and urethral plate | Penile urethra/ventral penis | Labia minora |
| Labioscrotal folds | Scrotum | Labia majora |
DEVELOPMENT OF THE REPRODUCTIVE SYSTEM – SUMMARY
- Development of the Gonads
- Indifferent stage
- Ovary: primary cords disappear. Cortical cords from germinal epithelium become primary follicles.
- Testis: tunica albuginea separates sex cords from the germinal epithelium. Sex cords become seminiferous tubules and rete testis. Germinal epithelium becomes the peritoneum. Interstitial cells develop. Connection to mesonephric system established.
- External Genitalia
- Female: genital tubercle becomes clitoris. Urogenital folds become labia minora leaving urethral opening in U.G. sinus. Labioscrotal folds fuse posteriorly, forming posterior labial commissure, and anteriorly, forming mons pubis. The central unfused portions are the labia majora. Urogenital sinus remains as vestibule of vagina.
- Male: genital tubercle becomes glans. Urogenital folds become incorporated into ventral portion of penis as urethral groove, which closes proximal to distal, enclosing the urethra. Labioscrotal folds fuse along length to form scrotum.
- Descent of Gonad
- Female: gubernaculum guides descent. Interrupted by broad ligament, so that ovary comes to rest on posterior surface of broad ligament. Proper ligament of ovary and round ligament of uterus are remnants of the gubernaculum.
- Male: tunica vaginalis enters scrotum and prepares a home appropriate for testis to function. Testis descends into scrotum guided by gubernaculum, behind peritoneal process. Canal obliterates.
- Developmental Disorders
- Sex Determination occurs at three levels:
- Chromosomal – Whether XX or XY
- Gonadal – Whether testis or ovary
- Phenotypic – Whether male or female.
- Sex Determination occurs at three levels:
In normal development there is a concordance between the three. In abnormal development, there may be mismatching between chromosomal sex and phenotypic sex. Sex assignment is made on the basis of the anatomy of the external genitalia. While this is the most easily identifiable criterion for sex, it is the least reliable.
- Hermaphroditism
- Pseudohermaphroditism
- Klinefelter & Turner syndromes
- Anomalies of uterus
- Defective partitioning of cloaca
Embryology of the reproductive System quiz click here