16 Autonomic Nervous System and Thorax Structure List
Autonomic Nervous System
Learning Objectives
- Describe the basic anatomical differences between the parasympathetic and sympathetic components of the autonomic nervous system, including the location of their pre- and post-ganglionic ganglia and neurotransmitters involved
- Predict the effects that lesions of the parasympathetic and sympathetic systems components have on different organs
- Describe the paths which splanchnic nerves take as they pass from the central nervous system to their target organs
- Interpret the phenomenon of dermatomal referred pain on the body surface in light of the general concept of visceral afferent fibers which travel along autonomic nerve pathways.
Reference for Autonomic System of Thorax and Abdomen: Moore, Clinically Oriented Anatomy, p. 58 – 66, 118-119, p. 148-149, p. 301-305
Particularly relevant Blue Boxes in Moore:
● Angina Pectoris p. 156
● Cardiac Referred Pain, p. 159
To access the Netter Presenter Database click here
The Autonomic Nervous System
Introduction
Definition: Those neurons, nuclei, ganglia and plexuses of the central and peripheral nervous systems that are involved in the innervation of structures concerned with involuntary actions (e.g., smooth muscle, cardiac muscle and glands)
The autonomic nervous system is concerned with those processes normally beyond voluntary control and beneath consciousness. It maintains the consistency of the body’s internal environment while buffering it against external or internal forces threatening to cause variation in this environment.
The autonomic nervous system is not readily dissectible because its neurons are intermingled with those that serve other functions. A two neuron chain is employed by the ANS to carry impulses from the central nervous system to the effector organs. The dendrites and cell body of the first neuron are in the central nervous system (CNS) and its axon leaves the CNS to synapse with a second neuron lying outside the CNS in the peripheral nervous system (PNS). The dendrites and cell bodies of the second neuron are generally clumped into autonomic ganglia. The axon of the first neuron in the chain is referred to as the preganglionic fiber while that of the second neuron is called a postganglionic fiber.
The two divisions of the ANS are the sympathetic and parasympathetic. The sympathetic division has preganglionic cell bodies located in the thoracic and upper lumbar regions of the spinal cord (T1-L2/3). Its preganglionic fibers are short and its postganglionic fibers are long. The parasympathetic division has preganglionic cell bodies located in the brainstem and sacral region of the spinal cord. Its preganglionic fibers are long and postganglionic fibers are short. In both divisions, the preganglionic fibers are usually mylinated whereas the postganglionic fibers are not.
Most of the effector organs of the ANS are innervated by both the sympathetic and parasympathetic division. The parasympathetics are distributed mostly to the thoracic, abdominal and pelvic viscera and to smooth muscle and glands in the head. However, blood vessels and sweat glands receive only sympathetic innervation.
Stimulation of the sympathetic division results in a diffuse outburst of activity in the course of fight and flight. Examples are increased blood flow to cardiac and striated muscle (increased expenditure of energy) and decreased blood flow to the GI tract (conservation of energy). Stimulation of the parasympathetic division results in effects that are localized. Examples are slowed heart beat (conservation of energy) and increased peristalsis of the GI tract (acquisition of energy stores)
Acetylcholine (ACh) is the mediator of impulses at all preganglionic synapses in the ANS, all postganglionic parasympathetic terminations, and postganglionic sympathetic endings at sweat glands and blood vessels to skeletal muscle. Cholinergic is a term used to describe liberating acetycholine. Norepinephrine (NE) is the mediator of impulses at the remaining postganglionic sympathetic endings. Adrenergic is a term used to describe nerves liberating norepinephrine.
Adrenal Gland
Chromaffin cells are found in the adrenal medulla and qualify as “neurons” because they are derived from neural crest cells. The chromaffin cells therefore serve as the second element in the sympathetic chain (i.e., like postganglionic neurons). Therefore when sympathetic preganglionic fibers, located in the medulla, release ACh as neurotransmitter, the chromaffin cells respond by secreting epinephrine and norepinephrine directly into the blood stream for sympathetic distribution.
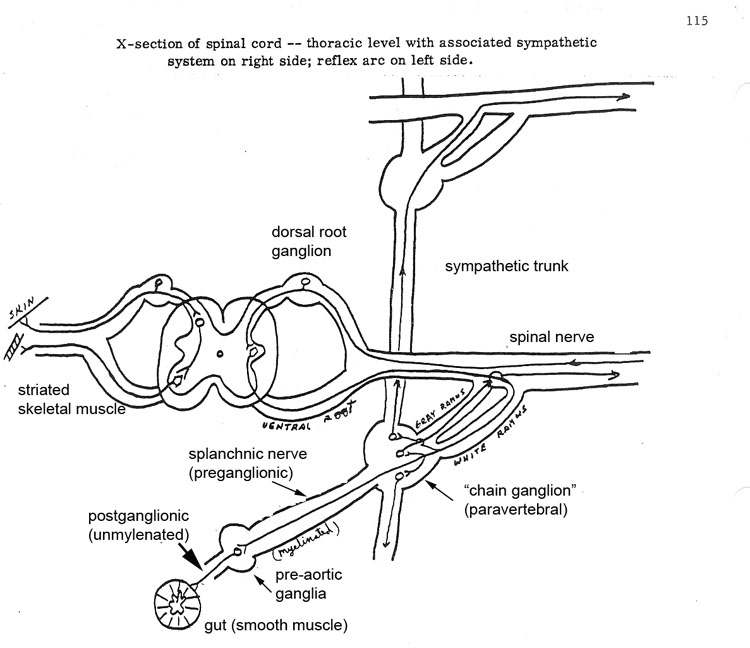
There are 31 segments of the spinal cord. The left side represents 31 spinal nerves, one for each cord segment. For simplicity sake, the right side represents the sympathetic components. One must realize, however, that the human body is actually bilateral with respect to both. Thus the diagram represents:
1. The spinal cord with 31 pairs of spinal nerves
2. 14 white rami communicantes – arising from the spinal cord between T1 and L2; these white rami communicantes contain preganglionic axons which pass to
3. 31 gray rami communicantes exit from a total of 19 – 22 paravertebral “chain” ganglia. The superior, middle and inferior cervical ganglia lie in the neck region, 14 ganglia lie along the lateral border of the vertebral column in relation to T1 to L2; and several ganglia lie in lower abdominal and pelvic regions. All of these ganglia are inter-connected by the sympathetic trunk. Thus the cervical ganglia receive preganglionic fibers from upper thoracic levels and the pelvic ganglia and lower abdominal ganglia receive preganglionic fibers from lumbar and lower thoracic segments.
- Splanchnic* nerves (greater, lesser and least) comprised of preganglionic fibers from levels T5 through T12 pass without synapse through the chain to pre-aortic ganglia (celiac, renal, superior mesenteric); synapses occur in these ganglia and the postganglionic fibers form nerve plexuses on the surface of blood vessels, passing to organs to be innervated.
5. Each spinal nerve receives postganglionic axons through gray rami communicantes from the paravertebral ganglia
* Splanchnic – associated with the viscera, as opposed to somatic – to those structures which developed from somites (e.g. muscles, skin)
Sympathetic Nervous System
Described as Thoraco-lumbar – preganglionic cell bodies are located in intermediolateral cell columns of spinal cord between levels T1 and L2/L3.
|
Activity of sympathetic system (conservation of energy)
|
This portion of the ANS takes precedence during activity, which could be thought of in terms of “fight or flight” situations, in other words, emergency.
General Visceral Efferent/Motor (GVE)
Preganglionic cell bodies are located in the intermediolateral cell column of the spinal cord between levels T1 and L2-3. (There are no preganglionic sympathetic cell bodies found at any other cord level). The preganglionic fiber exits the spinal cord and gains access to the postganglionic cell body by traversing the following course:
1. Ventral root
2. Spinal nerve
3. Ventral primary ramus
4. White ramus communicante
5. Sympathetic chain
Postganglionic cell bodies are located in sympathetic ganglia. There are two major categories of sympathetic ganglia:
1. Para-vertebral or sympathetic chain ganglia
2. Pre‑vertebral (preaortic)
The sympathetic chain (Netter 206) , and its associated paravertebral ganglia, is a paired structure lying on the lateral border of the vertebral column. The first three ganglia found in cervical regions are named the superior, middle and inferior cervical ganglia, respectively. None of the other ganglia are named and generally are about 22 total (including the 3 cervical). Each ganglion between levels T1 and L2/3 is connected to a corresponding spinal nerve by two communicating branches called gray and white rami communicantes. The function of the white rami communicantes is to allow preganglionic (generally myelinated, hence “white”) fibers access to the sympathetic chain. Since preganglionic fibers only originate in the spinal cord between T1 and L2/3, white rami communicantes can only be found at these levels. The function of the gray ramus is to allow postganglionic fibers (generally unmyelinated hence “gray”) an opportunity to exit the sympathetic chain and gain access to a spinal nerve that distributes it with all of its branches. Gray rami are found at all cord levels.
Once the preganglionic fibers enter the sympathetic chain, they have four options (Netter 225):
1. Synapse with a postganglionic neuron within the paravertebral ganglion.
2. Ascend within the sympathetic trunk to synapse with a postganglionic neuron within a paravertebral ganglion at a higher vertebral level.
3. Descend within the sympathetic trunk to synapse with a postganglionic neuron within a paravertebral ganglion at a lower vertebral level.
4. Pass through the paravertebral ganglion at that level without synapsing to reach a prevertebral ganglion (Netter 303, 304).
Preganglionic sympathetic fibers destined for the head, neck, thorax, extremities and body wall will take options 1-3 listed above. The sympathetic fibers traveling to the head ascend to synapse in the superior cervical ganglion and the postganglionic fibers travel along arteries or cranial nerves to reach their target. This will be covered in more detail in the ANS II lecture. The sympathetic fibers traveling to the thoracic viscera (heart, lungs, and esophagus) arise from levels T1-T5 and either synapse within the paravertebral ganglion at that level or ascend to the middle or inferior cervical ganglia to synapse. The postganglionic sympathetic fibers pass through cardiopulmonary splanchnic nerves to reach their target organs (Netter 224).
Preganglionic fibers destined for the abdomen or pelvis will take option 4. Prevertebral ganglia are collections of postganglionic cell bodies surrounding the major arterial branches of the abdominal aorta. Preganglionic fibers leave the spinal cord by the ventral root, ventral primary ramus and gain access to the sympathetic chain via a white ramus communicante. The preganglionic fibers pass through the ganglion and then leave the sympathetic chain as abdominopelvic splanchnic nerves. Most splanchnic nerves, carrying preganglionic fibers, pass posterior to the diaphragm to enter the abdominal cavity and synapse on postganglionic cell bodies in the prevertebral ganglia. These splanchnic nerves are called the greater, lesser, and least splanchnic nerves. The greater splanchnic nerve carries preganglionic sympathetic fibers from T5 – T9, the lesser splanchnic nerve carries fibers from T10-11, and the least splanchnic nerve carries fibers from T122. There are also lumbar splanchnic nerves that carry preganglionic sympathetic fibers from L1 -L3, but do not travel posterior to the diaphragm because they arise from vertebral levels below the diaphragm. The postganglionic fibers are then distributed to the abdominal and pelvic viscera by following periarterial plexuses associated with branches of the arterial system. NOTE: There is an exception to the rule with sympathetic innervation to the adrenal (suprarenal) gland. The preganglionic sympathetic fibers destined for the adrenal medulla do not synapse in a prevertebral ganglion. Instead, they travel through the ganglion and terminate on suprarenal medullary cells, which function as specialized postganglionic neurons. These cells release adrenaline directly into the bloodstream, producing a widespread sympathetic response.
Parasympathetic Nervous System
This system is describes as “cranio sacral” because its preganglionic neurons originate in the brain and sacral regions. It predominates during normal activity, thus maintaining homeostasis. Frequently spoken of as “rest and digest” rather than “fight or flight”.
|
Activity of the parasympathetic system:
|
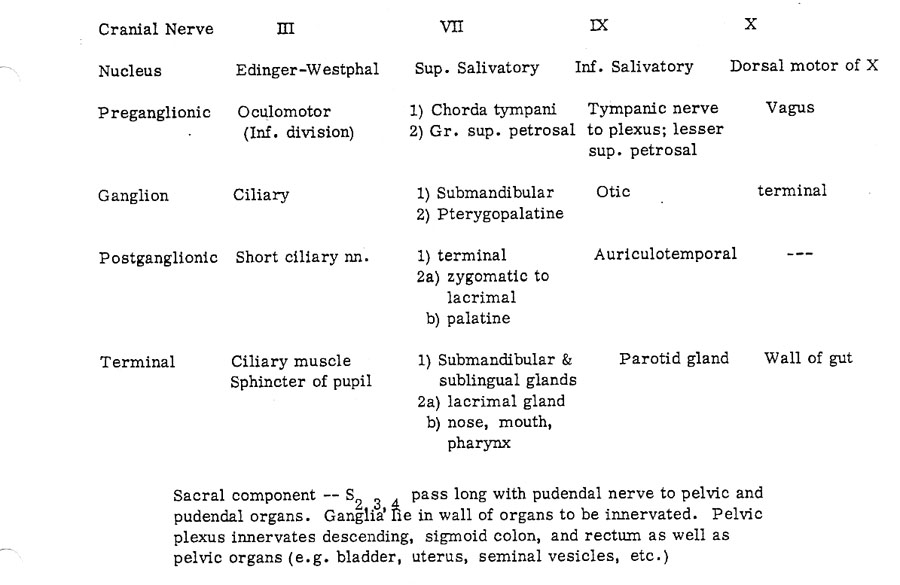
The following table summarizes the parasympathetic system
General Visceral Efferent/Motor (GVE)
Preganglionic parasympathetic cell bodies are located in two places within the CNS: the brainstem (cranio-) and the sacral region of the spinal cord (-sacral). The cell bodies within the brainstem are called brainstem nuclei and are associated with cranial nerves (CN) III, VII, IX, and X – oculomotor (III), facial (VII), glossopharyngeal (IX), and vagus (X). The preganglionic parasympathetic fibers within these cranial nerves are also known as the cranial parasympathetic outflow. The cell bodies in the gray matter of the spinal cord lie within the intermediolateral cell column at levels S2-4 and are also known as the sacral parasympathetic outflow. CN III, VII, and IX carry preganglionic parasympathetic fibers to the head and will be covered in more detail in the ANS II lecture. CN X carries preganglionic parasympathetic fibers to the thoracic and most of the abdominal viscera (through the left colic flexure of the large intestine). Preganglionic parasympathetic fibers from S2-4 pass through pelvic splanchnic nerves to the distal portion of the large intestine, pelvic viscera, and reproductive organs.
Postganglionic parasympathetic cell bodies receiving the cranial parasympathetic outflow from CN III, VII, and IX lie within four ganglia in the head (ciliary, submandibular, pterygopalatine and otic) to be covered in ANS II. Ganglia associated with sacral and CN X outflow are found in the walls of the organs to be innervated and are called enteric ganglia (Auerbach’s and Meissner’s enteric ganglia being examples).
Sympathetic nervous system
● Diverts blood flow away from the gastro-intestinal (GI) tract and skin via vasoconstriction.
●Blood flow to skeletal muscles, the lung is not only maintained, but enhanced (by as much as 1200%, in the case of skeletal muscles).
●Dilates bronchioles of the lung, which allows for greater alveolar oxygenexchange.
●Increases heart rate and the contractility of cardiac cells (myocytes), thereby providing a mechanism for the enhanced blood flow to skeletal muscles
●Dilates pupils, allowing more light to enter the eye.
Parasympathetic nervous system
●Dilates blood vessels leading to the GI tract, increasing blood flow. This is important following the consumption of food, due to the greater metabolic demands placed on the body by the gut.
●The parasympathetic nervous system can also constrict the bronchiolar diameter when the need for oxygen has diminished.
●During accommodation, the parasympathetic nervous system causes constriction of the pupil and lens.
●The parasympathetic nervous system stimulates salivary gland secretion, and accelerates peristalsis, so, in keeping with the rest and digest functions, appropriate PNS activity mediates digestion of food and indirectly, the absorption of nutrients.
●Is also involved in erection of genitals, via the pelvic splanchnic nerves 2–4.
Thoracic splanchnic nerves (Netter 299, 304, ) arise from the sympathetic trunk in the thorax and travel inferiorly to provide sympathetic innervation to the abdomen. The nerves contain preganglionic sympathetic and visceral afferent fibers.
There are three main thoracic splanchnic nerves:
| Name | Ganglia | Description |
| greater | T5-T9 | The nerve travels through the diaphragm and enters the abdominal cavity, where its fibers synapse at the celiac ganglia. The postganglionic nerve fibers contribute to the celiac plexus, a network of nerves located in the vicinity of where the celiac trunk branches from the abdominal aorta. These fibers modulate the activity of the enteric nervous system of the foregut. |
| lesser | T10-T11 | The nerve travels inferiorly, lateral to the greater splanchnic nerve. Its fibers synapse on postganglionic sympathetic cell bodies mostly in the superior mesenteric ganglion. These fibers modulate the activity of the enteric nervous system of the midgut. |
| least or lowest | T12 | The nerve travels into the abdomen, where its fibers synapse in the aorticorenal ganglia. The postganglionic sympathetic fibers modulate the activity of the kidneys, adrenal glands, and gonads. |
| The Cervical Portion of the Sympathetic and Parasympathetic System | ||
| The cervical portion (Netter 224, 131 ) of the sympathetic trunk consists of three ganglia, distinguished, according to their positions, as the superior, middle, and inferior ganglia, connected by intervening cords. This portion receives no white rami communicantes from the cervical spinal nerves; its spinal fibers are derived from the white rami of the upper thoracic nerves, and enter the corresponding thoracic ganglia of the sympathetic trunk, through which they ascend into the neck. After synapsing in these ganglia, they give off superior, middle and inferior cardiac nerves which descend into the thorax to provide sympathetic innervation to the trachea, esophagus, larynx, lungs and heart. The parasympathetic portion of the cardiopulmonary plexus is provided by the vagus nerve (cranial nerve X). Visceral afferent (sensory) nerves accompany the sympathetic fibers back to dorsal root ganglia associated with spinal cord levels T1 – T4, giving referred pain to these dermatomes during, for example, cardiac ischemia or myocardial infarction.The Cardiac Plexus (Netter 223) receives the superior, middle and inferior cervical and thoracic cardiac nerves from the sympathetic trunks and vagus nerves. It is divisible into the superficial cardiac plexus, which lies beneath the arch of the aorta, in front of the pulmonary artery, and the deep cardiac plexus, which lies posterior to the arch of the aorta, in front of the bifurcation of the trachea. The cardiac plexus innervates the conducting system of the heart: the right sympathetic and parasympathetic branches end chiefly in the region of the SA node and the left branches end chiefly in the region of the AV node. The cardiac muscle fibers are devoid of motor endings and are activated by the conducting system. It also supplies the heart with sympathetic fibers, which increase the heart rate and the force of the heartbeat, causing dilation of the coronary arteries and parasympathetic fibers which decrease the heart rate. | ||
Autonomic Nervous System quiz click here |
||
Osteology
Thoracic inlet, outlet
Sternum
Manubrium
Body
Sternal angle
Xiphoid process
Ribs
Costochondral junction
Head
Body
Angle
Tubercle
Costal groove
Thoracic vertebrae
Facets for ribs
Thoracic Wall
Intercostal muscles
External
Internal
Innermost: transversus thoracis, subcostalis
Vessels and nerve of thoracic wall
Internal thoracic artery: divides into:
Musculophrenic .
Superior epigastric a
Anterior and posterior intercostal arteries
Intercostal nerves (Ventral primary rami of thoracic spinal nerves)
Lungs and Pleurae
Costal, diaphragmatic and mediastinal pleurae
Bare area of pericardium
Costodiaphragmatic recesses
Pulmonary ligament
Lungs
Cupola
Hilus (root): secondary brinchi, pulmonary arteries and veins, bronchial arteries, lymph nodes
Right lung
Superior, middle and inferior lobes
Oblique and horizontal fissures
Azygous impression
10 bronchopulmonary segments (no need to memorizes names of these segments)
Left Lung
Superior and inferior lobes
Lingual
Cardiac notch
Aortic impression
10 bronchopulmonary segments
Heart and Pericardium
Fibrous pericardium
Transverse pericardial sinus
Oblique pericardial sinus
Atrioventricular (coronary) sulcus
Interventricular sulcus
Right, left auricles
Right coronary artery
SA nodal branch
Right marginal branch
AV nodal branch
Left coronary artery
Anterior interventricular (LAD) branch
Circumflex branch
Left marginal branch
Great cardiac vein
Middle cardiac vein
Coronary sinus
Right atrium
Crista terminalis
Musculi pectinati
Fossa ovalis
Limbus fossa ovalis
Opening for coronary sinus
Tricuspid valve
Right ventricle
Trabeculae carnae
Papillary muscles (anterior, posterior, septal)
Moderator band (septomarginal trabecula)
Chordae tendinae
Infundibulum
Pulmonic semilunar valve
Left atrium
Openings for pulmonary veins
Mitral valve
Left ventricle
Myocardium
2 papillary muscles and chorda tendinae
Aortic semilunar valve
Mediastinal Structures
Right, left brachiocephalic veins
Superior vena cava
Aorta
Ascending
Arch – branches:
Brachiocephalic trunk
Left common carotid a.
Left subclavian a.
Descending
Pulmonary trunk
Right, left pulmonary arteries
Ligamentum arteriosum
Azygous system of veins
Azygous vein
Hemiazygous vein
Accessory hemiazygous vein
Esophagus
Thoracic duct
Phrenic nerves
Right and left vagus nerves
Left recurrent laryngeal nerve
Sympathetic trunks
White and gray rami communicantes (you probably cannot distinguish these on the cadaver)
Greater splanchnic nerves
Esophageal plexus