17 Week 13: Altered Mental Status (Week of 12/11/2023)
Week 13: Altered Mental Status
DISCUSSION SESSIONS Week of 12/11/2023
Assignments Due: 12/12/2023 @ 8 AM
Prior to Class
- Read syllabus section on altered mental status (below)
- Complete the required quiz (Quiz L) on Canvas.
- Complete pre-class case, Mr. Seaver.
- Prepare answers to discussion questions on pre-class cases (emailed when case opens on Canvas).
Learning Objectives
- Describe the assessment of illness severity.
- Build a prioritized differential diagnosis for altered mental status that includes common and life/function threatening diagnoses.
- Identify the key history, physical exam, laboratory, and radiological findings that are useful in the evaluation of patients with altered mental status.
Assessing Illness Severity
A fundamental skill in patient evaluation and the development of a differential diagnosis is the rapid initial assessment of a patient, in which one hopes to glean the patient’s stability and the severity of their illness. This rapid assessment, sometimes called the eyeball test, consists of two key components—the patient’s general appearance and vital signs.
General Appearance
A patient’s general appearance is the first thing that should be noted when a physician enters the room, as this can set the tone for the entire encounter. With practice, you should be able to gather a large amount of information in a few seconds. Most individuals can evaluate whether a person is not sick, moderately sick, or very sick just by looking at them. At this stage in your clinical career, it will be beneficial to start developing a vocabulary for how to describe a patient’s general appearance concisely. The list below gives some examples of information that an experienced clinician can ascertain by simply observing a patient. You should work on observing these features in patients you see during clinical exposures.
- General distress, e.g. sweating, anxiety, fidgeting
- Build, e.g. obesity, cachexia, appearing different from chronological age
- Pain, e.g. grimacing, labored movements, patient’s position, gait
- Respiration, e.g. rate, rhythm, accessory muscle use
- Neurologic presentation, e.g. coordination, gait, weakness
- Psychiatric presentation. e.g. interaction, confusion, mania, flat affect, agitation
- Trauma, e.g. burns, wounds, bleeding
Vital Signs
The vital signs are straightforward markers of disease. Signs that raise suspicion of a severe illness that needs to be rapidly evaluated include:
- Fever (>38.0° C) or hypothermia (<36.0°C)
- Hypertension (SBP ≥ 160) or hypotension SBP (< 90)
- Tachypnea (RR ≥ 20) or bradypnea (RR ≤6)
- Tachycardia (HR > 100) or bradycardia (HR < 45)
- Hypoxia (O2Sat ≤ 92%)
Approach to Altered Mental Status
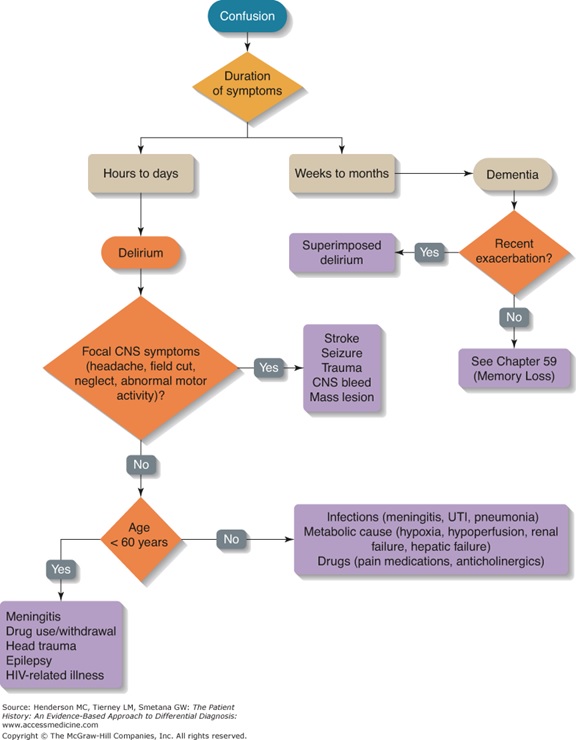
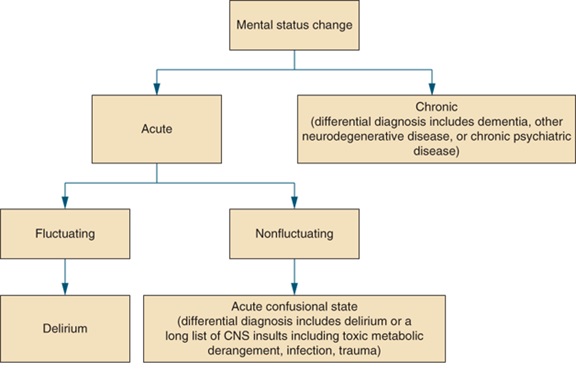
Altered mental status may be chronic or acute. Chronic confusion is typically called dementia, while the technical term for acute confusion is delirium. Delirium is defined as a disturbance of consciousness with reduced ability to focus, sustain, or shift attention that is not better explained by dementia. Symptoms of delirium develop rapidly, over hours to days, and tend to vary throughout the day. The key ways to distinguish delirium from dementia are duration of confusion and the waxing and waning nature of the symptoms with delirium. Also dementia does not cause a change in level of alertness (e.g., somnolence, stupor), so if these are present in a patient with dementia, they likely have both dementia AND delirium.
It is important to remember that delirium is a medical illness caused by a somatic condition or intoxication. It may present as the only sign of an underlying medical condition or as an adverse reaction to a drug. Precipitating factors to keep in mind include:
- Infection
- Fever
- Medication side effects
- Intoxication
- Postoperative states (especially 2-7 days’ post-op)
- Metabolic disorders – electrolyte imbalance, dehydration, increased or decreased glucose, renal failure, hepatic failure
- Cardiopulmonary disorders – CHF, MI, shock, pulmonary emboli
- Hypoxia, hypercapnia
- Sleep deprivation
- Use of physical restraints
- Use of bladder catheters
- Neurological/CNS disorders
An Algorithmic Approach to Altered Mental Status
Resources for Further Reading
- Harrison’s Principles of Internal Medicine, “Confusion and Delirium”
- UpToDate, “Diagnosis of delirium and confusional states”
