12 Week 9: Weakness (Week of 10/9/2023)
Week 9: Weakness
DISCUSSION SESSIONS Week of 10/9/23
Assignments Due: 10/10/2023 @ 8:00 AM
Prior to Class
- Read syllabus section on weakness (below).
- Complete the required quiz (Quiz H) on Canvas.
- Complete pre-class case, Mrs. Dryden.
- Prepare answers to discussion questions on pre-class cases (emailed when case opens on Canvas).
Learning Objectives
- Define asthenia and differentiate it from neuromuscular weakness.
- Build a prioritized differential diagnosis for a patient presenting with neuromuscular weakness that includes common and life/function threatening disorders.
- Identify the key findings of the history, physical exam, laboratory tests, and radiological studies for a patient with neuromuscular weakness.
- Compare and contrast the diseases on the differential diagnosis using illness scripts, specifically determining what symptoms, signs, and data findings differentiate one disease from another.
Evaluating Weakness
The first step in evaluating a patient with weakness is to determine what a patient means when saying they feel weak. Many patients who complain of weakness are suffering from functional weakness, also known as asthenia, which is defined as a sensation of weakness despite the presence of normal muscle strength. Asthenia is very common (nearly everyone experiences it at some point) as it is global and non-specific weakness on the basis of an underlying illness. In contrast, true neuromuscular weakness is the inability to move muscles at full strength despite maximum effort. This is usually due to an issue with muscle control or contraction. Weakness may also refer to increased fatigability of a patient’s muscles with repetitive movements or limited mobility despite full muscle strength secondary to pain. Furthermore, patients may describe feeling weak due to combinations of these causes, making evaluation very challenging. Therefore, in the initial history, it is important to attempt to distinguish asthenia from neuromuscular weakness.
Differentiating Asthenia from Neuromuscular Weakness
Patients with asthenia often describe feeling “wiped out” or “run down”. It is a subjective, generalized weakness usually resulting from a systemic problem, such as infection, metabolic derangement, inflammatory disease, cancer, or psychiatric disorder. With asthenia, patients will often describe having trouble completing activities of daily living because of a lack of physical or emotional energy. A detailed history and physical exam, however, will demonstrate normal muscle function and strength.
In addition, patients with asthenia are more likely to have symptoms and/or signs that suggest a systemic illness (e.g., fever, weight loss, abnormal vital signs). A detailed history is necessary to localize other features of the underlying disease and to guide next steps. The physical exam in patients with asthenia is unremarkable other than findings secondary to the underlying disease.
Evaluating Neuromuscular Weakness
Patients with true neuromuscular weakness have demonstrable weakness of specific muscle groups. One key factor that makes true neuromuscular weakness more likely is the reported inability to perform specific tasks, such as combing one’s hair, rising from a sitting position, or picking up objects.
The differential diagnosis of neuromuscular weakness is extensive. Using knowledge of the physiology of muscle contraction assists in organizing the differential. It is useful to recall the five steps in muscle contraction listed below:
- Initiation and propagation of a nerve impulse through the brain and spinal cord along the upper motor neuron
- Junction between upper motor neuron and lower motor neuron at the anterior horn cells
- Propagation down the lower motor neuron to the neuromuscular junction
- Junction between the lower motor neuron and the muscle at the neuromuscular junction (with acetylcholine as the neurotransmitter)
- Contraction of the muscle itself
Defects at any of these levels can cause neuromuscular weakness. A couple of other key things are worth keeping in mind,
- The cranial nerves innervate the facial muscles and include a motor neuron although there is no anterior horn cell involved. Anterior horn cells only reside in the spinal cord (i.e. the cranial nerve nuclei serve as the equivalent of the anterior horn cells).
- The post-ganglionic neurotransmitter in the parasympathetic nervous system is acetylcholine and thus problems that hit the neuromuscular junction also have the potential to hit these synapses. The sympathetic nervous system uses norepinephrine in its post-ganglionic synapses.
Weakness Alarm Symptoms
The table below lists serious and benign causes of symptoms related to weakness.
| Table. Muscle Weakness, Adapted from Muscle Weakness, Chapter 13. Iris Ma, MD. Copyright © McGraw-Hill Global Education Holdings, LLC. | ||
| Alarm Symptoms | Serious Causes | Benign Causes |
| Rapidly progressive descending paralysis | Botulism
Spinal cord compression (e.g. neoplasm, infection, trauma) Organophosphate poisoning |
|
| Rapidly progressive ascending paralysis | Guillain-Barre Syndrome | |
| Sudden onset hemiparesis | TIA
Stroke Intracranial Hemorrhage |
Hemiplegic Migraine
Conversion Disorder |
| Sudden onset monoparesis | TIA, Stroke, Mononeuropathy | Compressive Neuropathy |
| Localized back pain with paralysis | GBS
Spinal cord compression (e.g. neoplasm, infection, trauma) Transverse myelitis |
|
| Weakness seems to be transmissible | Botulism
Organophosphate poisoning |
|
| Diplopia, blurry vision, or bulbar symptoms with developing tetraparesis | Botulism
Organophosphate poisoning Brainstem stroke Multiple Sclerosis |
|
| Radicular pain (electric pain that follows a spinal root distribution) with paraparesis | Transverse myelitis
Spinal cord compression |
|
| Headache with hemiparesis | Intracranial bleed
CNS malignancy Brain abscess |
Hemiplegic migraines |
| History of heavy exercise or repetitive activities | Rhabdomyolysis | Compressive neuropathy
Exertional fatigue |
| History of cancer | Metastatic disease
Paraneoplastic syndromes |
|
| History of fevers or injection drug use | Epidural abscess | |
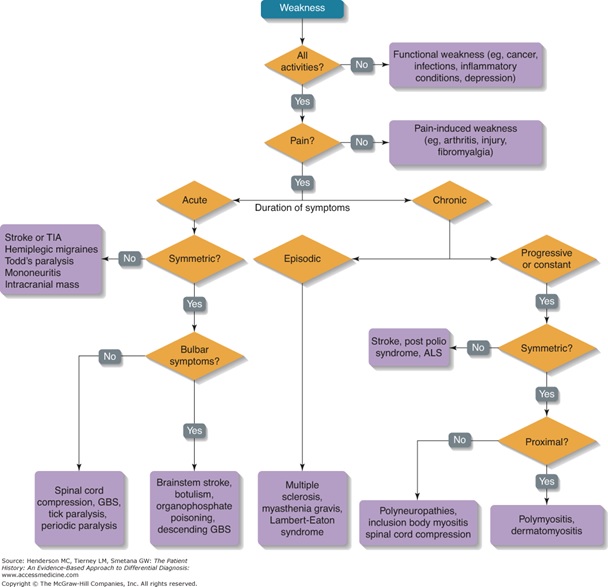
An Algorithmic Approach to Weakness
The algorithm below provides an approach to considering the differential diagnosis for weakness.
Resources for Further Reading
- UpToDate, “Approach to the patient with muscle weakness”
