6 Week 4: Fever in a Child (Week of 4/15/2024)
Week 4: Fever in a child
DISCUSSION SESSIONS WEEK OF 4/15/24
Assignments Due: 4/16/2023 @ 8:00AM
PRIOR TO CLASS
- Watch Canvas video on thresholds.
- Read syllabus section on fever in a pediatric patient (below).
- Complete the required quiz (Quiz C) on Canvas.
- Complete pre-class case, Addie Davis.
- Prepare answers to discussion questions on the pre-class case (emailed when case opens on Canvas).
Learning Objectives
- Describe the use of thresholds to test and thresholds to treat
- Describe the approach to fever in a pediatric patient
- List the common and life/function threatening causes of fever in pediatric patients of specific ages
- Build a differential diagnosis for a pediatric patient presenting with fever that includes common and life/function threatening diseases
- Identify the components of the history and physical, as well as the laboratory and radiological findings, crucial for correctly diagnosing a pediatric patient presenting with fever.
THRESHOLDS TO TEST AND TREAT
The threshold to test is a level of disease probability below which no further testing is necessary for that disease. It is determined through considering the risks and benefits of testing versus not testing for the specific disorder.
| Factors that decrease the threshold to test | Factors that increase the threshold to test |
| High disease morbidity/mortality | Low disease morbidity/mortality |
| Low risk test | High risk test |
| Excellent test performance | Marginal test performance |
As an example, consider whether to test for disease X. Let’s assume that X has a high mortality rate and the test for X is both low risk and highly accurate (e.g. low false positive rate, low false negative rate). Because of the high mortality rate and availability of a low risk and highly accurate test, we would set the threshold to test very low. An example of such a test would be an electrocardiogram (ECG) to diagnose acute coronary syndrome (ACS). Untreated ACS poses a significant morbidity and mortality risk. An ECG is very low risk and highly accurate. Therefore, in the case of a potential ACS, our threshold to test would be very low. This concept is represented graphically below.
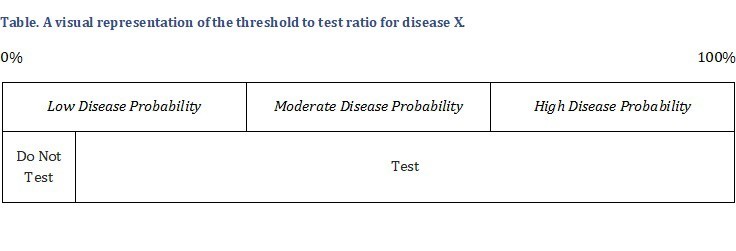 Thus, even when the probability of disease is somewhat low, most doctors would still test for X. If the test is negative, it may allow them to lower the disease probability to one below the threshold to test. In determining whether a negative test would actually do this, we could find the likelihood ratios for the proposed test and see if a negative test results in a post-test probability below the threshold to test.
Thus, even when the probability of disease is somewhat low, most doctors would still test for X. If the test is negative, it may allow them to lower the disease probability to one below the threshold to test. In determining whether a negative test would actually do this, we could find the likelihood ratios for the proposed test and see if a negative test results in a post-test probability below the threshold to test.
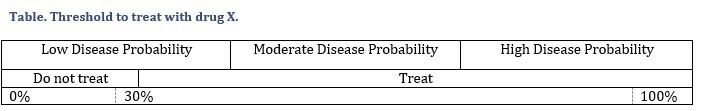
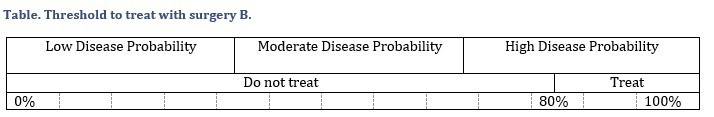
The threshold to treat is the clinical probability of a disease above which treatment is thought reasonable. It is determined by a calculation of the relative risks and benefits of treating versus not treating a patient for that specific disease.
| Factors that decrease the threshold to treat | Factors that increase the threshold to treat |
| High disease morbidity/mortality | Low disease morbidity/mortality |
| Low risk treatment | High risk treatment |
| Effective treatment | Less effective treatment |
As an example, consider a disease with significant mortality that has a treatment that is highly effective and poses little risk. In this case, we will likely initiate treatment even if the probability of disease is relatively low (for example 30%). This is graphically depicted below. An example of this would be treatment of coronary artery disease with aspirin.
On the other hand, if treatment of the disease incurs substantial risk, such as surgery, or the treatment is not very effective, the threshold to treat is higher and it would take a probability of, for example, 80% before we use the treatment. This is depicted below.
We rarely calculate these numbers mathematically in a clinical setting; instead, we use the concepts intuitively to make sure that we are thinking about disease probability and the risks and benefits of testing and treating before making decisions regarding our patients. An important qualifier to this is that the thresholds may vary from patient to patient. We may, for example, have a higher threshold to test in a patient in whom the test has a higher likelihood of harm, such as a CT with intravenous contrast in a patient with significant kidney disease (similarly, the threshold to test is higher when the test is less accurate). Or we may have a higher threshold to treat a patient with anticoagulation for a pulmonary embolism if the patient has a history of recurrent severe gastrointestinal bleeding. All of this makes the setting of thresholds a difficult and somewhat moving target.
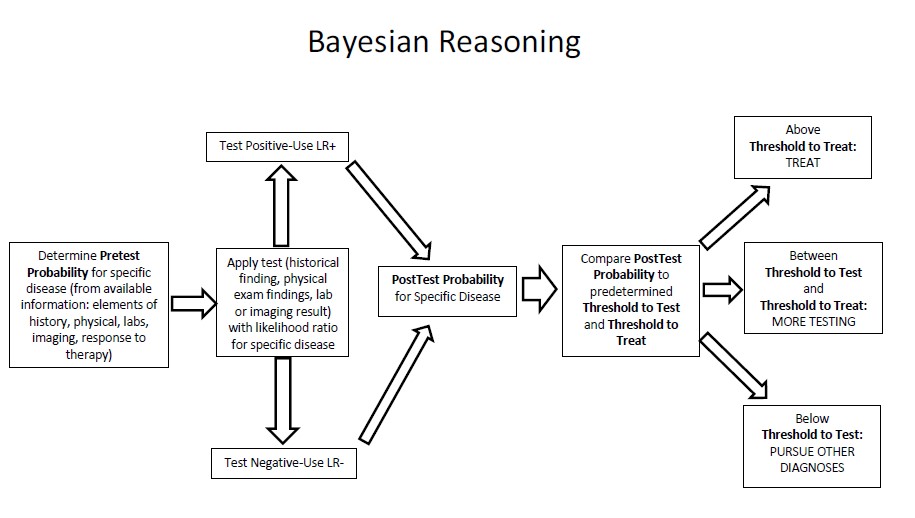
PUTTING IT ALL TOGETHER: A REVIEW OF BAYESIAN ANALYSIS
Bayesian analysis is an iterative step-wise process that involves determining a pre-test probability, subjecting that pre-test probability to a test, and comparing the resultant post-test probability to the thresholds to test and treat. Clinical findings and tests may be applied serially in Bayesian analysis, so long as the tests are independent of one another. Using Bayesian analysis in calculating probabilities of disease may seem daunting, but it is a crucial ability to develop.
STEP ONE: DETERMINING THE PRE-TEST PROBABILITY OF A DISEASE
This may be derived from epidemiological data or from the results of prior testing. It is known, for example, that of patients presenting to outpatient centers with chest pain, as many as 12% of them are found to have coronary disease. Without knowing any other data, our pre-test probability of coronary artery disease of such a patient is 12%. Gaining data such as exacerbating and relieving factors, age, and sex would alter this probability.
We then look to see if the pre-test probability of disease falls between the thresholds to test and treat. If the probability is below the threshold to test, no testing is necessary and we should move on to considering other diagnoses. If the probability is above the threshold to treat, we should treat. A test should only be done if the probability of the disease is between the two thresholds (usually the threshold to test on the lower end and the threshold to treat on the higher end).
STEP TWO: APPLYING THE LIKELIHOOD RATIO
It is important to apply a likelihood ratio (LR) for each test** the patient is subjected to. Each test has a positive LR that we use when the test is positive and a negative one that we use when the test is negative. We thus use the positive LRs for the symptoms/signs/lab/radiology findings a patient has and the negative ones for the ones a patient doesn’t and apply them serially (as long as they are independent tests) to arrive at a post-test probability for the specific disease. Independent tests are tests whose results don’t rely on similar modalities of testing.
A helpful online calculator for post-test probability at “http://araw.mede.uic.edu/cgi-bin/testcalc.pl“.
(**In this instance, a “test” can refer to symptom, component of the history, physical finding, laboratory test, or imaging study.)
STEP THREE: APPLY THE THRESHOLDS OF DIAGNOSIS
When the threshold to treat (the upper threshold) is reached, we initiate treatment. When the probability of disease is below the threshold to test we discard the diagnosis and move on to considering other diagnoses. Often the post-test probability lies between the upper and lower thresholds. In this case, further testing should be performed.
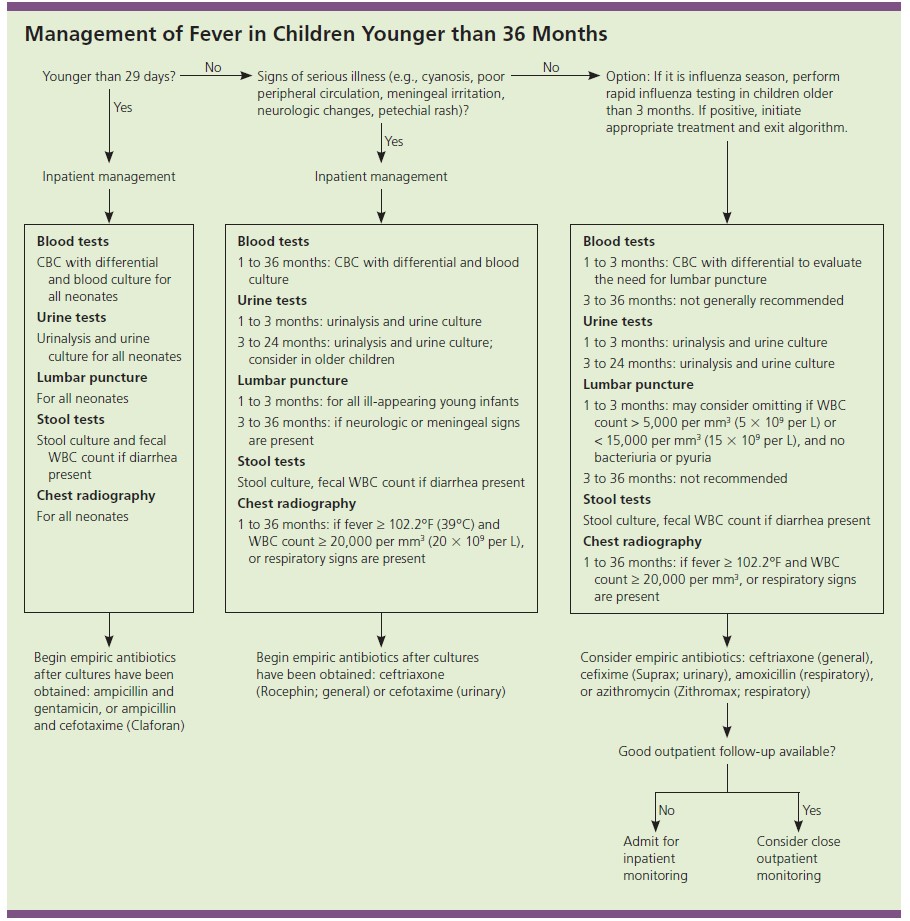
DIFFERENTIAL DIAGNOSIS FOR A nonspecific CONCERN SUCH AS FEVER
Basic epidemiologic data and patient characteristics can have a major effect of the differential diagnosis of a patient presenting with fever. An excellent example of this is the age of the patient. Although there is not much difference between the likely infections in a 25 year old versus a 45 year old despite the 20 year age difference, in children, even relatively small differences in age can profoundly affect the potential diagnoses. The etiology and evaluation of infants under the age of three months, for example, varies from that of a child 3 to 36 months in age. Even the temperature that is considered to constitute a fever may vary across age groups.
Using a construct such as VINDICATE (see Glossary of terms) can be very useful in helping to build a comprehensive differential diagnosis for patients presenting with fever and other broad symptoms. Repeatedly formulating extensive differential diagnoses for common clinical presentations helps to build the basis for future pattern recognition (non-analytic thinking). Pediatricians can seemingly effortlessly list the likely infections present in children of specific ages because they have run through these differentials many times. You should aspire to be able to do the same.
HISTORY-TAKING IN PATIENTS WITH FEVER
In evaluating a patient with an acute, subacute, or chronic fever, taking an appropriately detailed history is the most important diagnostic step. In a patient with acute fever, infection is the most likely diagnosis. Because the source of the infection may not be immediately apparent to the patient or physician, taking a comprehensive history is critical. Infection is also a common cause of sub-acute fever. Subacute fever can also be caused by auto-immune disorders, inflammatory disorders, and malignancy. Finally, in the case of chronic fever, malignancy, auto-immune diseases, and inflammatory conditions are more likely than infection, although the latter is still possible. It can’t be emphasized strongly enough that obtaining a good history is one of the most important aspects of the diagnostic evaluation. The diagnosis can be established on the basis of the history alone in upwards of 70% of patient presentations. This is particularly true in the patient presenting with fever. Listed below are vital components of the history for a patient who presents with fever.
Personal History
It is important to consider the epidemiology of diseases where a patient has lived in the past. For example, tuberculosis exposure is much more common in some countries than others.
SOCIAL HISTORY
A detailed social history may reveal a potential cause of fever. For example, a thorough sexual history and substance-use history may reveal risk factors for HIV. Immunosuppression secondary to HIV infection can predispose to other infections that cause fever and other symptoms.
OCCUPATIONAL HISTORY
In adults, exposure to various substances in the workplace is associated with many disease processes. Two examples that may cause fever are exposure to beryllium and organic dusts. Beryllium is used in the manufacturing industry and can cause berylliosis, a disease characterized by chronic granulomatous inflammation. Early symptoms include cough, dyspnea, chest pain, joint aches, weight loss and fever. Organic dusts can cause hypersensitivity pneumonitis which manifests principally as dyspnea and cough, and less commonly fever, chills, malaise, and chest tightness.
TRAVEL HISTORY
Travel can increase the likelihood of parasitic and protozoal infections, as well as many bacterial and viral diseases. Visiting or living in certain areas within the United States are correlated with a higher possibility of endemic mycoses. As an example, the Mississippi River Valley is associated with histoplasmosis while Arizona and the Central Valley of California are associated with coccidiomycosis.
FAMILY HISTORY
A family history of autoimmune diseases, inflammatory disorders, or malignancies may increase the likelihood of these diseases in the patient of interest.
PHYSICAL EXAMINATION OF A PATIENT WITH FEVER
Just as you will tailor the questions in taking a history in a patient with an acute concern, you will tailor what aspects of the physical examination you will perform. This can be particularly important in children; you need to know what to look for in order to find it. You are seeking defining features with high sensitivity that must be present to diagnose a disease and discriminating features with high specificity that help distinguish one disease from another. The absence of a defining feature may make a disease unlikely and the presence of a discriminating feature increases the likelihood of a disease.
Even small amounts of clinical information may result in the generation of new diagnostic hypotheses or refinement of prior diagnostic hypotheses. Although it may be difficult to make a diagnosis with scant information, small bits of information can have an effect on your differential diagnosis and determine which diagnostic path you elect to pursue. This is why a good exam is important in identifying a source of fever; an infection can be “hiding” nearly anywhere and looking everywhere may be necessary to find it.
WORST CASE SCENARIO
It is always worth consciously considering the “worst case scenario” in evaluating patients with fever. Urinary tract infection, pneumonia, osteomyelitis, meningitis, and bacteremia are the most common serious causes of fever due to infection in children. In patients under the age of three months, UTI is the most common serious bacterial infection. In patients aged three months to three years, pneumonia is most common serious bacterial infection followed by UTI. In neonates, additional considerations include omphalitis (infection of the umbilical stump) and mastitis.
That said, most patients with fever do not have the worst case scenario and we always need to explicitly consider the most common causes of fever. Acute otitis media is the most common bacterial infection in children but, in general, it is not a serious infection in the vast majority of patients. Serious infection can occur when the child is very young, is immunocompromised, or has craniofacial abnormalities (e.g., cleft palate). Viral respiratory infections (including RSV, rhinovirus, human metapneumovirus, and influenza) and bronchiolitis are other common causes of fever to consider.
RESOURCES FOR FURTHER READING
- Harrison’s Principles of Internal Medicine, “Fever”
- UpToDate, “Fever in infants and children: Pathophysiology and management” https://www.uptodate.com/contents/fever-in-infants-and-children-pathophysiology-and-management?search=fever&source=search_result&selectedTitle=2~150&usage_type=default&display_rank=2
