5 Week 3: Acute Kidney Injury (AKI) (Week of 4/3/2023)
WEEK OF 4/3/2023
Assignments Due: 4/4/2023 @8:00 AM
Prior to Class
- Watch Canvas video lecture, “Likelihood Ratios”.
- Read syllabus section on AKI (below).
- Complete the required quiz (Quiz B) on Canvas.
- Complete pre-class case, Mr. Nichols.
- Prepare answers to discussion questions on pre-class cases (emailed when case opens on Canvas).
- Recommended podcasts: https://thecurbsiders.com/podcast/226 (listen beginning at 09:15); https://podcasts.apple.com/us/podcast/s2d-the-symptom-to-diagnosis-podcast/id1548809192 (AKI, Feb 3, 2021)
Learning Objectives
- Describe likelihood ratios and how they affect the post-test probability
- Build a prioritized differential diagnosis for a patient presenting with AKI that includes the common and life/function threatening causes.
- Identify the components of the history and physical, as well as the laboratory and radiological findings, crucial for correctly diagnosing a patient presenting with AKI
Likelihood ratios
Determining the likelihood, or probability, of diseases on the differential diagnosis is one of the critical skills of clinical reasoning. Probability is a mathematical term suggesting that diagnosis is a calculation but obviously bedside clinicians do not mathematically calculate the new probability of the diseases on their differential diagnosis every time they learn about a new clinical finding. They prioritize the probabilities as more likely or less likely based on a gestalt feeling that they get from the clinical findings that are present or absent. However, understanding how the math of clinical reasoning works can make you a better clinician because you’ll be a more thoughtful diagnostician. It will also allow you to know the key discrimination and differentiating aspects of the clinical exam when approaching a patient with a specific issue (i.e. what really matters to ask and look for). To understand the math, you need to understand likelihood ratios. This content was covered in EBM and is represented here as a review.
Likelihood ratios are simply a numerical expression of the strength of the association between a finding and a specific disease based on its sensitivity and specificity. The best way to understand the absolute value of a clinical finding is to calculate its likelihood ratio positive (LR +) and negative (LR −). Briefly, a positive LR is the true positive rate/false positive rate (sensitivity/ 1-specificity, where sensitivity = TP/TP+FN, and 1-specificity= FP/FP+TN) and a negative LR is the false negative rate/true negative rate (1− sensitivity/specificity, where 1−sensitivity= FN/TP+FN and specificity = TN/TN+FP). Thus, the higher the positive LR the better, (more true positives relative to false positives), while the lower the negative LR the better (less false negatives relative to true negatives). In applying likelihood ratios, you use the LR+ when the test is positive and the LR- when the test is negative.
Unfortunately, you can’t just multiply the pretest probability by the likelihood ratio to get the posttest probability as likelihood ratios are based on odds, not probabilities. Most people have a difficult time with odds (perhaps this is why Vegas makes a lot of money off people) whereas probabilities are more intuitive. So, in using likelihood ratios, you technically need to convert the probability to odds, multiple the odds by the likelihood ratio to get the post-test odds and then convert the post-test odds to the post-test probability. This is obviously cumbersome and confusing so most people just use the Bayes nomogram (which we will always supply when needed in the course) or an online calculator.
The table below gives you a rough idea of how various likelihood ratios affect the probability of disease (these are just estimates) and are very helpful to know:
As a reminder…
A positive LR of 2 mildly increases the disease likelihood.
A positive LR of 5 moderately increases the disease likelihood.
A positive LR of >10 significantly increases the disease likelihood.
A negative LR of 0.5 mildly decreases the disease likelihood.
A negative LR of 0.2 moderately decreases the disease likelihood.
A negative LR of <0.1 significantly decreases the disease likelihood.
Note: This estimation does not perform well at the extremes of pre-test probabilities.
Typical Patterns of Acute Kidney Injury
Perfusion-Related Injury
Perfusion-related AKI is most commonly caused by either volume depletion or decreased effective arterial volume. True volume depletion commonly occurs with vomiting, diarrhea, profuse sweating, bleeding, sepsis (with intravascular fluid moving out of the vasculature), or environmental exposures especially in the setting of poor oral intake. Diuretic therapy is another common cause of volume depletion. Disorders that cause decreased effective arterial volume include cirrhosis, congestive heart failure, and nephrotic syndrome.
Obstructive Injury
Obstructive AKI occurs when urinary flow is obstructed. Unilateral ureteral obstruction generally will not cause renal failure. There must be either bilateral obstruction, obstruction of a single functional drainage system (e.g, single working kidney), or obstruction at the level of the bladder or below (e.g., urethra, prostate) for renal function to be significantly compromised. Potential causes of obstructive kidney injury include malignancy with bilateral ureteral obstruction, bladder cancer, bladder outlet obstruction due to prostatic enlargement, urethral stricture, or conditions where the bladder musculature cannot contract properly (neurogenic bladder).
Intrinsic Renal Disease
Intrinsic renal disease is the most complicated of the three types of AKI, but it can be more easily understood by breaking it down further into interstitial, tubular, and glomerular etiologies.
Interstitial
Acute interstitial nephritis is the most common interstitial cause of AKI and often manifests as fever, rash, arthralgias, and pyuria after exposure to an offending agent, most commonly antibiotics.
Tubular
Acute tubular necrosis (ATN) can cause AKI and is most frequently associated with either an ischemic or toxic insult. Hypotension, even if short in duration, is usually present in ischemic ATN. Toxin-mediated ATN may be secondary to endogenous toxins (e.g. myoglobin in rhabdomyolysis, free hemoglobin in hemolysis) or exogenous toxins (e.g. aminoglycosides, amphotericin, cis-platinum, contrast dyes used for imaging studies).
Glomerular
Most of the glomerular causes of AKI are systemic diseases and have key elements of the history and physical examination that point to them as the etiology. Granulomatosis with polyangiitis, microscopic polyangiitis, eosinophilic granulomatosis with polyangiitis, and Goodpasture’s disease, for example, are pulmonary-renal syndromes that often have concomitant pulmonary involvement. Also, red blood cell casts and dysmorphic red blood cells in the urine sediment are very specific for glomerulonephritis.
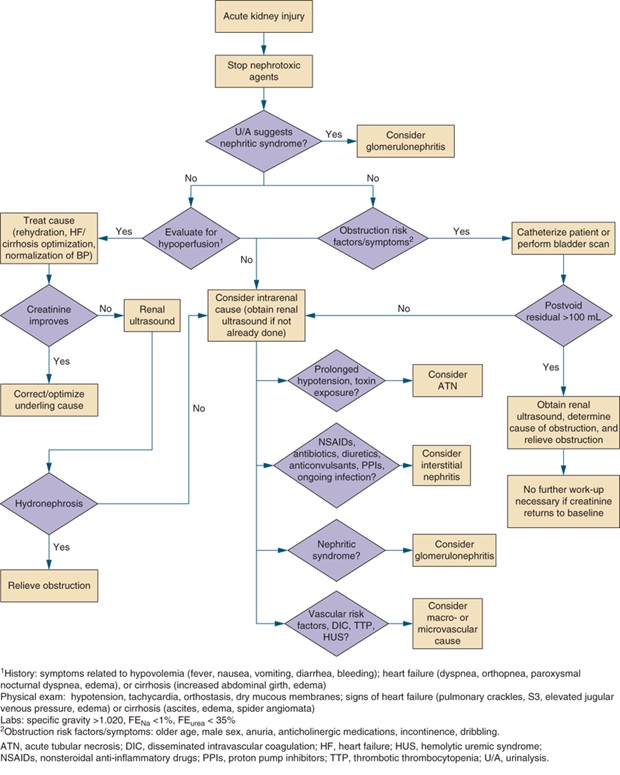
An Algorithmic Approach to AKI
Below is an algorithm that may be helpful when considering the differential diagnosis for AKI.
Resources for Further Reading
- Harrison’s Internal Medicine, “Acute Renal Failure”
- UpToDate, “Definition of acute kidney injury”
